Understanding the Importance of Managing Sugar Levels

How are you really managing your sugar levels? It’s a question worth asking, especially as we observe World Diabetes Day—a global call to rethink how we approach health, nutrition, and lifestyle. Blood sugar management isn’t just for those diagnosed with diabetes; it’s a cornerstone of well-being for everyone. Our energy, mood, focus, and even long-term health depend on stable glucose levels.
Think of your body as an engine. Glucose is your fuel, and insulin is the mechanism that helps your cells absorb it efficiently. When this process works smoothly, you have balanced energy and a strong immune system. But when things go wrong—too much glucose, too little insulin, or the body becoming resistant—the system breaks down.
The reality is that high blood sugar levels can silently damage your heart, kidneys, nerves, and eyes. What’s more concerning? Many people don’t even realize their sugar levels are out of balance until complications appear. This World Diabetes Day, it’s time to slow down and take stock. Are you checking your sugar regularly? Are your meals balanced, your sleep adequate, and your mind calm?
This article explores every aspect of managing sugar levels naturally—from food and exercise to mental health and awareness—so you can take control of your health journey.
Why World Diabetes Day Matters for Everyone

Every year on November 14, the world unites to spread awareness about diabetes, its prevention, and the importance of sugar management. But here’s the truth—World Diabetes Day isn’t just for those already living with diabetes. It’s for everyone, because nearly half of the adults with high blood sugar don’t know they have it.
The theme of this year’s campaign centers around rethinking our lifestyle and understanding that managing sugar levels is not a once-in-a-while task but a lifelong commitment. The growing prevalence of diabetes across the world tells a story of changing diets, sedentary habits, and stress.
We live in a fast-paced world fueled by processed foods and sugary drinks. Add lack of sleep and constant stress, and you’ve got the perfect recipe for unstable glucose. By reflecting on this day, we remind ourselves that prevention is better than cure. Managing sugar levels is the foundation of preventing diabetes and ensuring long-term vitality.
So, whether you’re young or old, active or sedentary, this day is a reminder: your sugar levels deserve your attention.
The Science Behind Blood Sugar Levels

What is Blood Sugar?
Blood sugar, or glucose, is the body’s primary source of energy. It comes from the food you eat, especially carbohydrates, which are broken down into glucose and absorbed into the bloodstream. The hormone insulin, produced by the pancreas, helps transport this glucose into cells to be used for energy or stored for later use.
When this system functions properly, your blood sugar levels remain stable. However, if your body produces little or no insulin—or your cells become resistant to it—glucose builds up in your blood. Over time, this can lead to diabetes or prediabetes.
How the Body Regulates Glucose
Your body is constantly working to keep blood sugar within a narrow range. After eating, insulin levels rise to help cells absorb glucose. When you haven’t eaten for a while, another hormone called glucagon signals the liver to release stored glucose.
This balance can be disrupted by poor diet, stress, illness, or lack of activity. Maintaining stable blood sugar levels means respecting this natural rhythm—by eating balanced meals, staying active, and managing stress.
Different Types of Diabetes and Their Impact on Sugar Levels
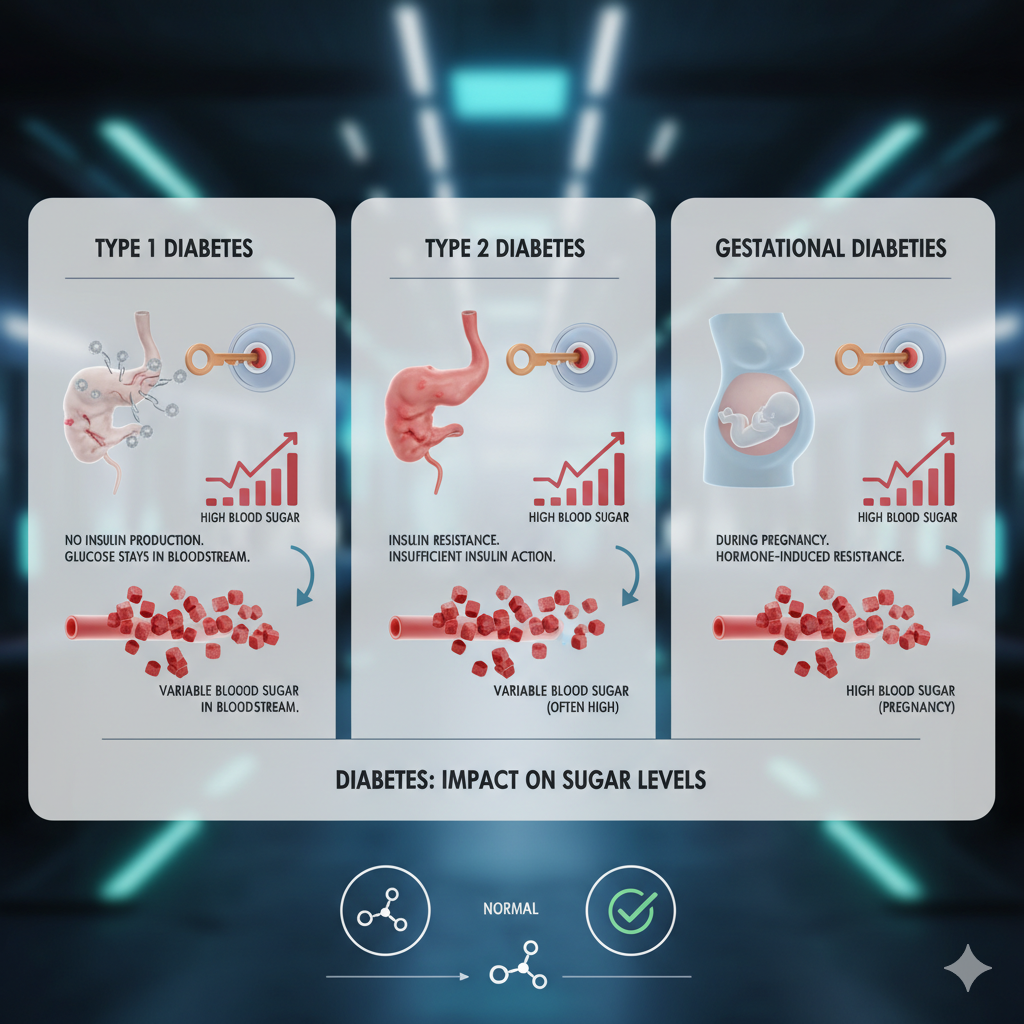
Type 1 Diabetes: The Autoimmune Challenge
Type 1 diabetes occurs when the body’s immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. People with Type 1 must rely on insulin injections or pumps to survive. Though it often develops in childhood, adults can be diagnosed too. Managing sugar levels here requires constant vigilance—monitoring food intake, exercise, and insulin dosage.
Type 2 Diabetes: The Lifestyle Connection
Type 2 diabetes is far more common and largely preventable. It develops when the body becomes resistant to insulin or doesn’t produce enough. Factors like poor diet, obesity, and inactivity play a huge role. The good news? With lifestyle changes—healthy eating, weight control, and regular physical activity—blood sugar can be managed and sometimes even reversed.
Gestational Diabetes: Managing Sugar Levels During Pregnancy
Gestational diabetes affects pregnant women when hormones interfere with insulin function. Though it usually disappears after childbirth, it increases the mother’s risk of developing Type 2 diabetes later. Regular monitoring, balanced nutrition, and gentle exercise are essential during pregnancy.
Early Warning Signs of Uncontrolled Sugar Levels
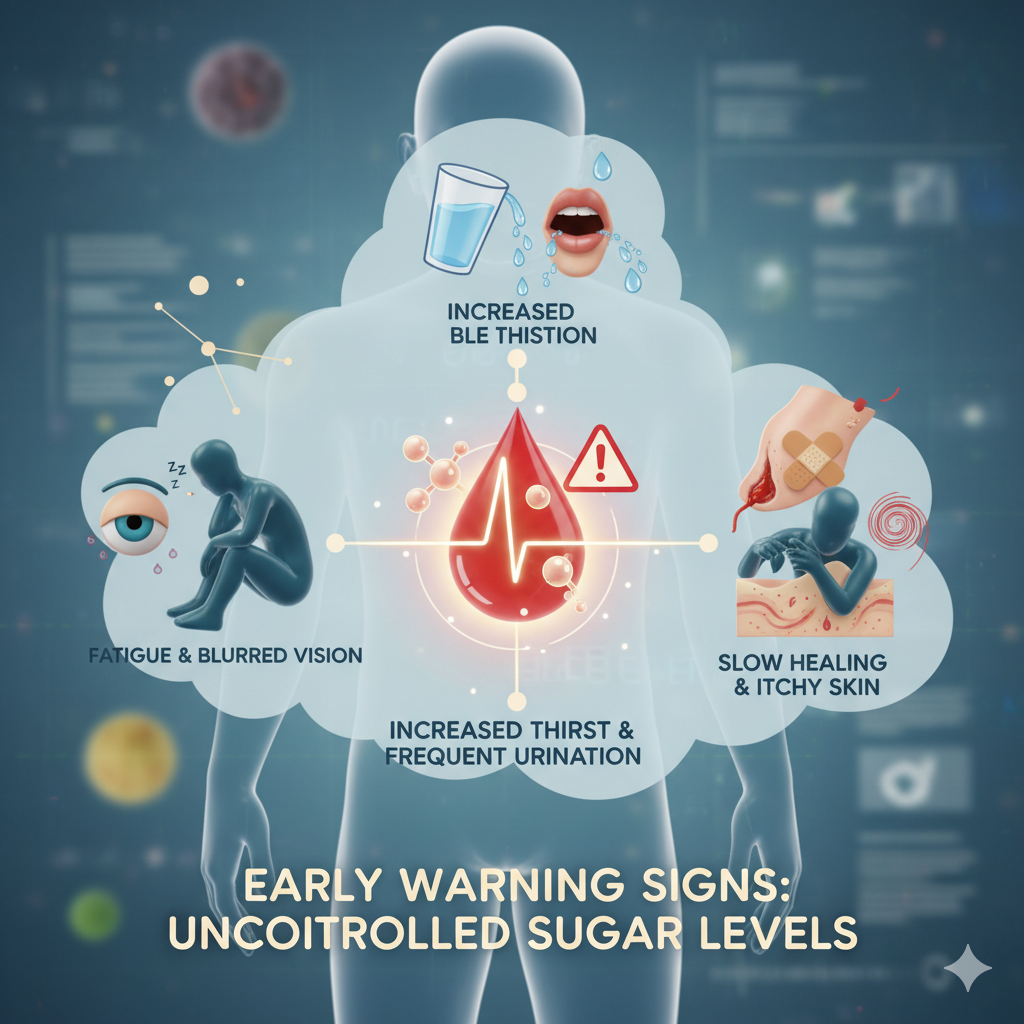
Unstable sugar levels don’t happen overnight—they build up gradually. Recognizing early symptoms of diabetes can save you from severe complications. Common signs include frequent urination, extreme thirst, unexplained fatigue, blurred vision, and slow healing of wounds.
These symptoms might seem harmless at first, but they’re your body’s way of signaling distress. Imagine your body as a finely tuned machine—when glucose levels rise beyond normal, every system starts working overtime. You may feel constantly thirsty because your kidneys are trying to flush out excess sugar. Fatigue creeps in because glucose, your main energy source, can’t efficiently enter your cells.
Some people also experience sudden weight changes, tingling sensations in their hands or feet, or recurring infections. These are all red flags of poor sugar control. What’s tricky is that early signs of high sugar can easily be mistaken for stress or tiredness. That’s why regular blood sugar checks are crucial, especially if you have a family history of diabetes or lead a sedentary lifestyle.
Prevention starts with awareness. If you experience any of these symptoms, don’t ignore them. Instead, get tested and discuss the results with a healthcare professional. Catching the issue early allows for timely management and prevents long-term damage to your organs.
How Diet Affects Sugar Levels and Overall Health
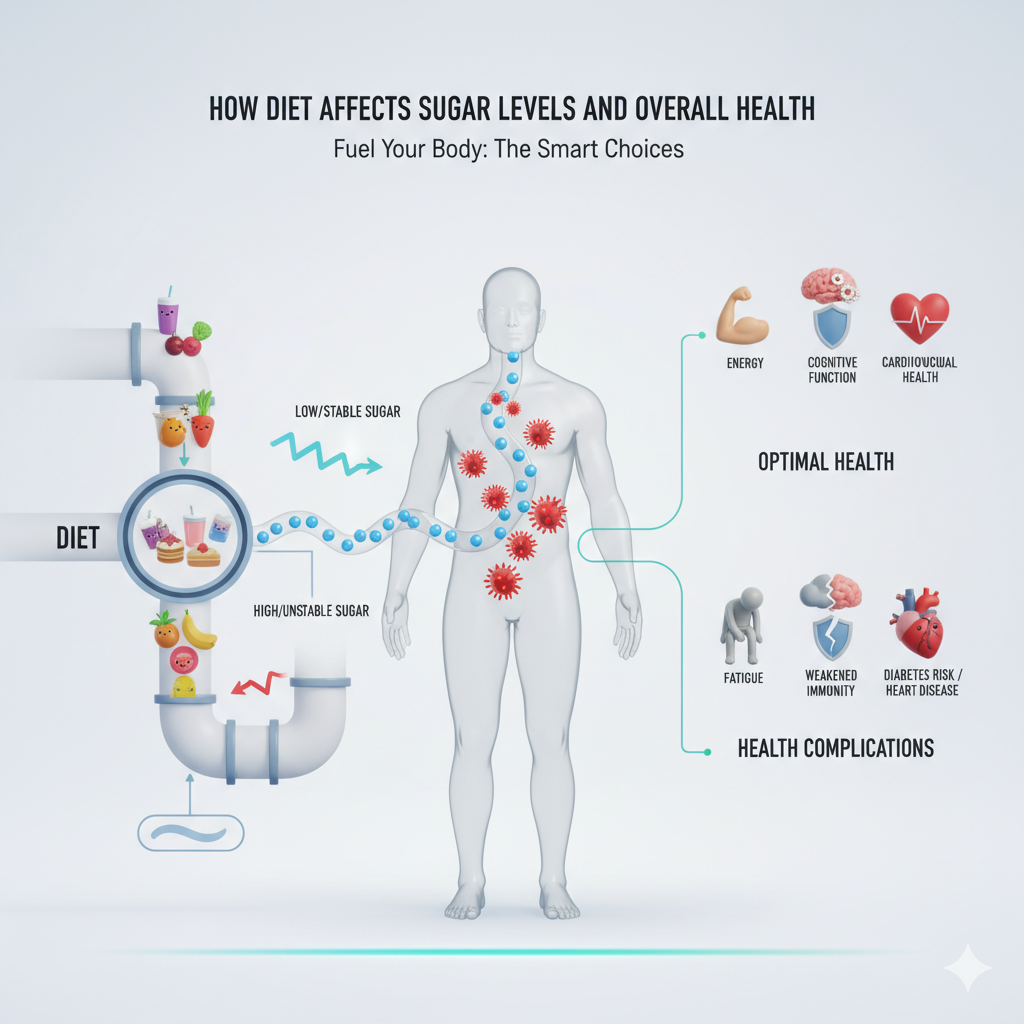
Diet plays a leading role in managing sugar levels—and it’s not just about cutting out sweets. Every meal you eat affects your blood glucose, depending on its nutrient composition. The three macronutrients—carbohydrates, fats, and proteins—each have a different effect on sugar levels.
The Role of Carbohydrates
Carbohydrates are broken down into glucose during digestion, making them the biggest influencers of blood sugar. However, not all carbs are created equal. Simple carbs like white bread, pastries, and sugary drinks spike your blood sugar quickly and then cause it to crash. Complex carbs like whole grains, legumes, and vegetables release glucose slowly, giving your body sustained energy without sharp spikes.
Understanding Glycemic Index
The Glycemic Index (GI) ranks foods based on how quickly they raise blood sugar levels. Low-GI foods (like oats, lentils, and sweet potatoes) release glucose gradually, keeping you full longer and maintaining energy balance. High-GI foods (like white rice and candy) can cause sudden glucose surges followed by energy crashes. Choosing low-GI foods is a powerful strategy to keep sugar levels stable throughout the day.
Smart Food Swaps for Balanced Blood Sugar
You don’t have to give up all your favorite foods; you just need smarter swaps. For example:
- Choose brown rice or quinoa over white rice.
- Replace soda with infused water or herbal tea.
- Snack on nuts and seeds instead of chips.
- Add fiber-rich vegetables to every meal.
Fiber slows down glucose absorption, while protein and healthy fats help balance your meal’s impact on sugar levels. Eating smaller, frequent meals rather than skipping and bingeing later also helps maintain stable energy. Remember: what you eat today determines how your body functions tomorrow.
The Power of Exercise in Managing Blood Sugar Levels
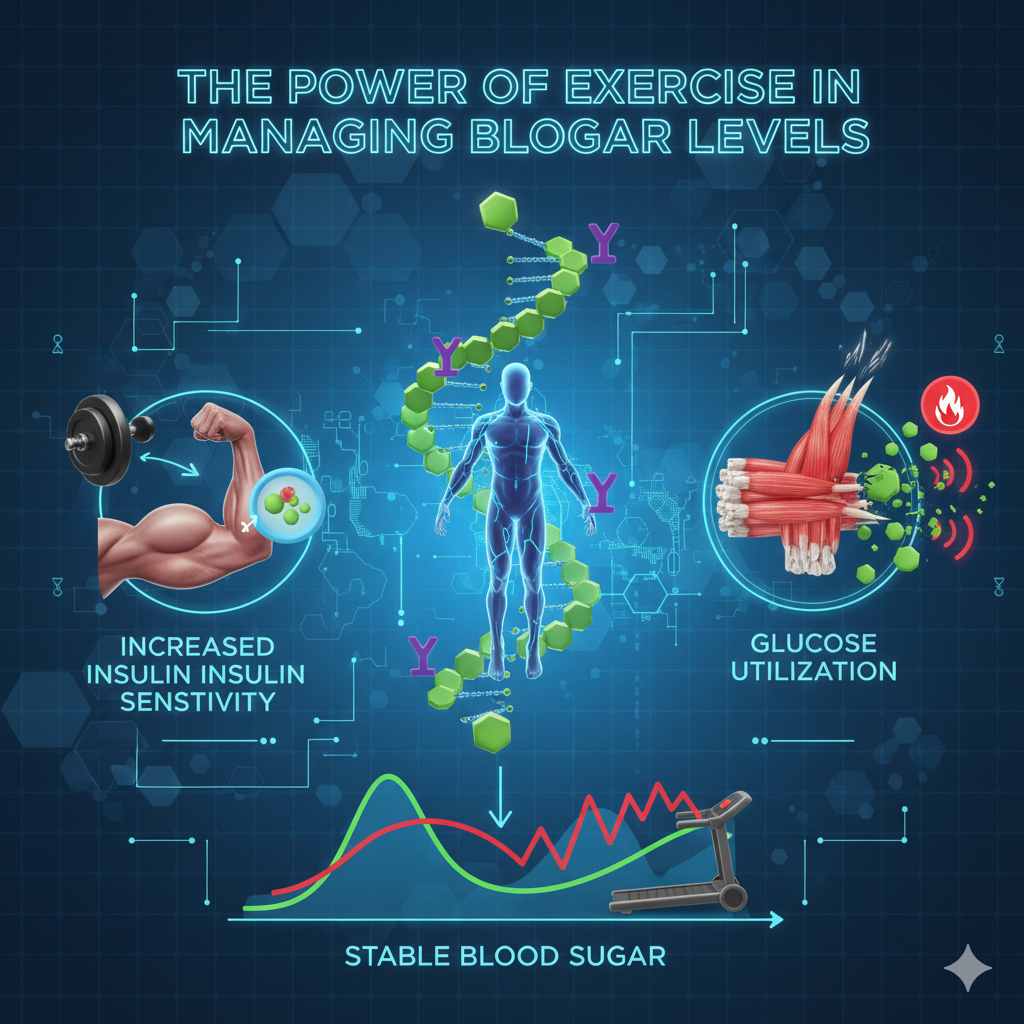
Physical activity is one of the most effective ways to manage sugar levels naturally. When you move, your muscles use glucose for energy, lowering blood sugar levels both immediately and in the long term. Regular exercise also improves insulin sensitivity, meaning your cells can use insulin more efficiently.
Best Types of Physical Activities for Diabetics
You don’t need to run marathons to improve your glucose control. Moderate activities like brisk walking, swimming, cycling, or dancing can make a huge difference. Strength training, such as lifting weights or using resistance bands, also helps by building muscle mass, which increases your body’s ability to absorb glucose.
How Consistency Beats Intensity
The secret isn’t intensity—it’s consistency. Even short bouts of movement throughout the day can stabilize blood sugar. A 15-minute walk after meals, for instance, can significantly reduce glucose spikes. The key is to stay active daily, whether that means taking the stairs, gardening, or doing yoga.
Simple Daily Movement Tips
- Stand up and stretch every hour if you have a desk job.
- Walk or cycle for short errands instead of driving.
- Try a 10-minute bodyweight workout every morning.
- Use a fitness tracker to monitor your steps and progress.
Exercise isn’t just about burning calories—it’s about balance. Regular movement improves mood, boosts energy, and strengthens your heart, making it an all-in-one health solution for sugar control.
Mental Health and Its Hidden Link to Sugar Control

Have you ever noticed that when you’re stressed, you crave sweets or feel drained? That’s not a coincidence—it’s biochemistry at work. Stress triggers the release of cortisol, a hormone that raises blood sugar to provide quick energy for “fight or flight.” But when stress becomes chronic, cortisol levels stay high, keeping your blood sugar elevated.
Stress and Cortisol’s Role in Glucose Spikes
When you’re under pressure—whether from work, finances, or personal struggles—your body produces cortisol to help you cope. Over time, constant stress can cause insulin resistance, making it harder for cells to use glucose effectively. This not only increases sugar levels but also leads to fatigue, irritability, and cravings.
Mindfulness Practices for Better Sugar Management
Managing stress is just as important as managing diet and exercise. Practices like meditation, deep breathing, and yoga calm the nervous system and lower cortisol levels. Even spending time in nature or doing creative hobbies can reduce stress hormones.
Try starting your day with five minutes of slow breathing or journaling before bed. Prioritizing mental well-being can improve physical health, too. After all, a calm mind supports a balanced body.
Sleep and Blood Sugar: The Overlooked Connection

When you skimp on sleep, your body doesn’t just feel tired—it becomes metabolically confused. Lack of sleep disrupts the hormones that regulate hunger and glucose. Ghrelin (the hunger hormone) increases, while leptin (the satiety hormone) decreases, causing you to crave sugary or high-carb foods.
How Poor Sleep Impacts Insulin Sensitivity
Research shows that even one night of poor sleep can make your body more resistant to insulin. This means your cells can’t use glucose efficiently, causing higher sugar levels the next day. Over time, chronic sleep deprivation increases the risk of obesity and diabetes.
Sleep Hygiene Tips for Better Sugar Levels
- Go to bed and wake up at the same time daily.
- Avoid caffeine or heavy meals before bedtime.
- Keep your bedroom dark, cool, and quiet.
- Limit screen time an hour before bed.
Good sleep is like a natural reset button for your body. By prioritizing 7–8 hours of restful sleep, you support hormone balance and healthier glucose levels.
Hydration and Its Role in Sugar Management
Water might not seem like a big player when it comes to managing sugar levels, but it’s a silent hero. When you’re dehydrated, your blood becomes more concentrated, causing sugar levels to appear higher. Proper hydration helps your kidneys flush out excess glucose through urine, maintaining balance naturally.
Why Water Matters
Water doesn’t just quench thirst—it regulates body temperature, supports digestion, and keeps blood sugar in check. People who drink enough water are less likely to experience glucose spikes, as hydration helps insulin work more efficiently. Think of water as your body’s natural detox mechanism.
The general guideline is to drink at least 8–10 glasses a day, but your needs may vary based on activity, climate, and diet. If you exercise often or live in a hot area, you’ll need even more. Herbal teas, coconut water, and lemon water are great low-calorie ways to stay hydrated.
Beverages to Avoid for Stable Sugar Levels
Not all drinks are created equal. Some beverages can quietly sabotage your sugar management goals. Here’s what to limit or skip:
- Sugary sodas – High in simple sugars and empty calories.
- Energy drinks – Contain excessive caffeine and hidden sugar.
- Packaged fruit juices – Even “no added sugar” labels can be misleading.
- Flavored coffee drinks – Often loaded with syrups and creamers.
Instead, opt for unsweetened tea, black coffee, or infused water with mint and cucumber. A small change in what you drink can have a massive impact on your blood sugar stability.
Monitoring Blood Sugar Levels Effectively

You can’t manage what you don’t measure. Regular monitoring of your blood sugar levels is one of the most empowering steps you can take toward better health. Tracking your glucose helps you understand how your body reacts to foods, stress, and activity.
Tools and Techniques for Self-Monitoring
There are two main ways to monitor sugar:
- Glucometers – Small, portable devices that require a drop of blood from your fingertip.
- Continuous Glucose Monitors (CGMs) – Wearable sensors that track sugar levels in real time.
By testing at different times—before and after meals, during exercise, or before bed—you can identify patterns. These insights allow you to make better food and lifestyle choices.
Understanding Your Numbers
Typical target blood sugar ranges for most adults are:
| Timing | Normal Range (mg/dL) |
| Fasting | 70–99 |
| 2 hours after eating | Less than 140 |
| Before bedtime | 100–140 |
However, these numbers may vary based on individual conditions. If you consistently notice high readings, it’s a signal to adjust your diet, exercise routine, or sleep habits. Tracking your sugar levels is not just about control—it’s about awareness.
Myths and Misconceptions About Managing Sugar Levels

When it comes to diabetes and sugar control, misinformation is everywhere. Let’s clear up some of the most common myths that might be holding you back from making the right decisions.
“Sugar Alone Causes Diabetes” and Other Myths
This is one of the biggest misconceptions. Eating sugar doesn’t directly cause diabetes—it’s a combination of factors like genetics, lifestyle, and body weight. However, excessive sugar intake can contribute to obesity, which increases the risk of Type 2 diabetes.
Another myth is that diabetics can’t eat fruits. In reality, fruits are full of vitamins, minerals, and fiber. The key is moderation and choosing low-glycemic options like berries, apples, and oranges instead of fruit juices.
The Truth About Artificial Sweeteners
Artificial sweeteners are marketed as “diabetes-friendly,” but the truth is more complex. Some people find them helpful in cutting down sugar intake, while others experience cravings or digestive discomfort. If you use them, do so in moderation and focus on whole, natural foods instead.
“Only Overweight People Get Diabetes”
While obesity is a major risk factor, even lean individuals can develop diabetes due to genetics or poor lifestyle choices. Everyone—regardless of body size—should be mindful of their sugar habits.
By understanding the truth behind these myths, you can make informed choices for your long-term health.
Preventing Diabetes Before It Starts

Prevention is always better than treatment. The best part? Type 2 diabetes is largely preventable through lifestyle changes that anyone can adopt. Managing sugar levels is not about strict diets or intense workouts—it’s about consistency and balance.
Lifestyle Changes for Long-Term Health
Start by reassessing your daily habits:
- Eat balanced meals with fiber, lean proteins, and healthy fats.
- Stay active for at least 30 minutes most days of the week.
- Limit processed foods high in refined carbs and added sugars.
- Get quality sleep to regulate hormones and appetite.
- Manage stress through meditation or physical activity.
These habits not only control sugar levels but also reduce your risk of heart disease, obesity, and hypertension.
Building Sustainable Habits
The trick to success is sustainability. Instead of trying to change everything overnight, focus on one small step at a time. Maybe start by reducing sugary drinks this week, adding 15 minutes of walking next week, and gradually building a healthy routine that lasts.
Remember, health isn’t a race—it’s a journey. Every positive action you take moves you closer to stable sugar levels and a stronger body.
Community Support and Awareness on World Diabetes Day

World Diabetes Day is more than an awareness event—it’s a reminder that change begins with collective action. Communities play a vital role in spreading education, breaking myths, and supporting those managing diabetes.
Families can encourage healthy meals at home, schools can promote active lifestyles, and workplaces can create wellness programs that prioritize movement and mindfulness. When people come together, the stigma around diabetes lessens, and understanding grows.
This day also calls for empathy. Living with diabetes can be overwhelming, but with support—from family, peers, or online communities—individuals can feel empowered to take control of their sugar levels. Awareness saves lives, and knowledge inspires healthier choices.
Rethinking Health: Making Sugar Management a Daily Habit
Managing sugar levels isn’t just something to think about once a year—it’s a daily commitment to a healthier lifestyle. The truth is, most people only start worrying about their glucose when health problems appear. But sugar balance should be part of our daily mindset, just like brushing our teeth or drinking enough water.
Integrating Small Changes for Big Results
You don’t need dramatic transformations to manage your sugar levels effectively. Small, consistent actions can create massive health benefits over time. Start with simple steps such as:
- Having breakfast every day to prevent sugar crashes later on.
- Including more vegetables in every meal for fiber and nutrients.
- Choosing homemade meals over processed or restaurant food.
- Taking a short walk after lunch or dinner to stabilize glucose.
- Checking your sugar levels once or twice a month even if you feel fine.
Each of these habits, while small individually, builds a powerful system for long-term sugar management. Think of them as daily deposits into your health account—steady, consistent, and always paying off in the long run.
Setting Realistic Health Goals
Many people struggle with health goals because they set unrealistic expectations. For example, aiming to lose 10 pounds in a week or cutting out all sugar instantly is rarely sustainable. Instead, set goals that are measurable and achievable.
Try something like:
- “I’ll reduce my sugary snacks from daily to twice a week.”
- “I’ll walk for 20 minutes after dinner every day.”
- “I’ll replace my afternoon soda with herbal tea.”
By setting attainable milestones, you build confidence and motivation. Remember, managing your sugar levels isn’t about perfection—it’s about progress. A slight improvement every week adds up to significant change over the course of months.
Making Health Enjoyable
The best way to stick with a lifestyle change is to enjoy it. Explore recipes for healthy desserts, experiment with herbal teas, or take a fun dance class instead of the treadmill. The goal is to associate sugar management with a positive experience, not a restrictive one.
When you approach your health journey with joy instead of fear, the process becomes more sustainable. World Diabetes Day serves as a reminder that living well isn’t about giving things up—it’s about choosing wisely and treating your body with kindness.
Take Charge of Your Sugar Levels This World Diabetes Day

So, how are you managing your sugar levels? This World Diabetes Day, take a moment to reflect—not with guilt, but with awareness. Every decision you make, from what you eat to how you move and sleep, affects your glucose balance.
Managing sugar levels isn’t just about avoiding diabetes; it’s about improving your quality of life. Stable blood sugar helps you stay energized, focused, and emotionally balanced. It protects your heart, preserves your eyesight, and keeps your mind sharp as you age.
The power is in your hands. Start today with one small change—swap that sugary drink for water, walk a little more, or take five deep breaths when stress hits. Over time, these small steps create a ripple effect that transforms your overall health.
World Diabetes Day is more than a campaign—it’s a global reminder that every action counts. So, let’s rethink health, one sugar-conscious choice at a time.
FAQs
1. How can I check my sugar levels at home?
You can use a glucometer or a continuous glucose monitor (CGM). A glucometer requires a small blood sample, while CGMs track sugar levels throughout the day via a sensor. Regular testing—especially before and after meals—helps you understand how different foods and activities affect your glucose.
2. What are the best foods to manage blood sugar naturally?
Focus on foods rich in fiber, lean protein, and healthy fats. Great choices include oats, whole grains, lentils, nuts, seeds, leafy greens, and non-starchy vegetables. These slow down digestion and prevent glucose spikes. Avoid refined carbs, sugary drinks, and highly processed foods.
3. Can stress really increase my sugar levels?
Yes! Stress triggers cortisol, a hormone that raises blood sugar levels. Chronic stress can make your body insulin-resistant. Practicing relaxation techniques like meditation, yoga, or even a short daily walk can help manage both stress and glucose.
4. How much exercise is enough for controlling sugar levels?
Aim for at least 150 minutes of moderate exercise per week, which breaks down to about 30 minutes a day, five times a week. Mix aerobic activities (like walking or swimming) with strength training for the best results.
5. Is it possible to prevent diabetes completely?
While genetics play a role, Type 2 diabetes is largely preventable. Maintaining a healthy weight, eating balanced meals, staying active, sleeping well, and managing stress can significantly reduce your risk. Prevention starts with awareness—and consistency keeps it strong.

Leave a Reply