Understanding Why Blood Sugar Rises During Winter
Winter feels cozy, but for many people struggling with high blood sugar, it can also be a troublemaker. The moment the temperature drops, the body begins behaving differently—sometimes in ways we don’t fully notice until the glucose meter shows a number that makes us raise an eyebrow. But why does this happen? The answer lies in how the human body naturally reacts to cold weather. When the temperature gets lower outside, the body tries to stay warm by using more energy. This often means it releases stress hormones such as cortisol and adrenaline. These hormones can make the liver release extra glucose into the bloodstream, which may cause higher blood sugar levels than usual.
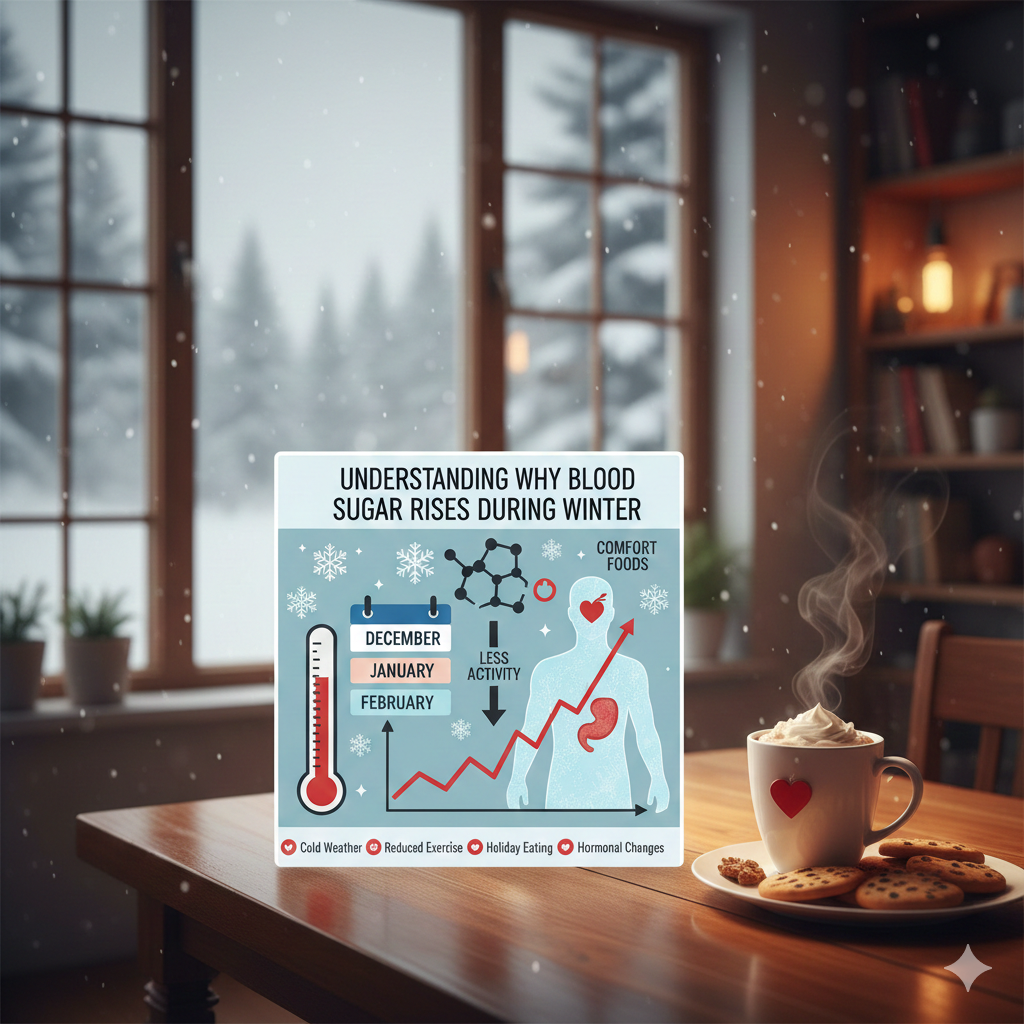
On top of that, winter often brings lifestyle changes we don’t pay enough attention to. People stay indoors more, they move less, and they tend to eat heavier, richer meals. Comfort foods like hot chocolate, creamy soups, and baked desserts become more tempting—and honestly, who hasn’t reached for a warm treat on a chilly night? These foods, though delicious, often have high amounts of sugar and carbohydrates, which push glucose levels higher. Without enough physical activity to balance this out, blood sugar can spike much faster than during warmer seasons.
Another overlooked factor is routine changes. Shorter daylight hours might mean waking up later, eating later, or sleeping more irregularly. These shifts can disrupt the body’s natural rhythm, affecting metabolism and glucose processing. The combination of less sunlight, lower activity, and heavier meals creates the perfect storm for blood sugar challenges. Understanding this connection is the first step in learning how to manage the winter roller coaster. Once you know the triggers, controlling your blood sugar becomes far easier, and winter becomes something to enjoy—not fear.
How Cold Weather Affects Insulin Sensitivity
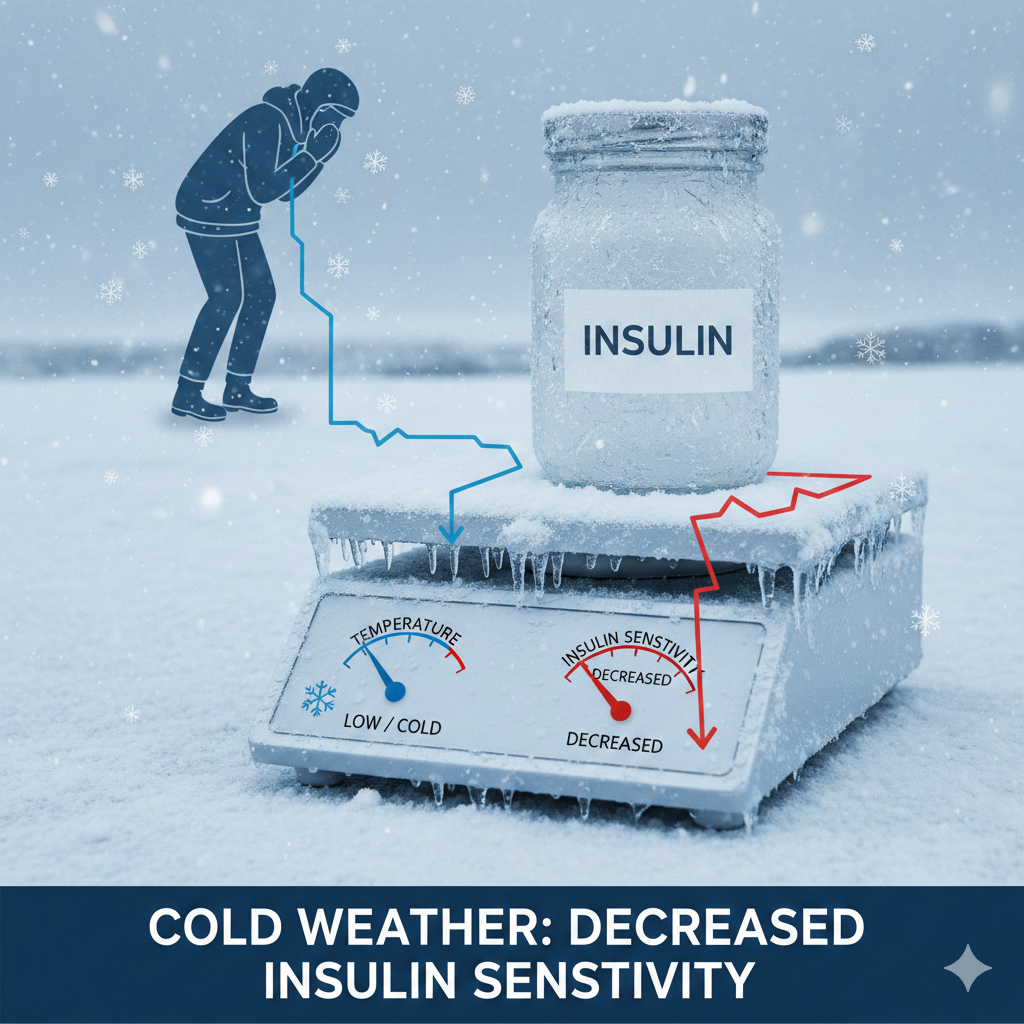
Cold weather doesn’t just make you shiver—it also changes the way your body uses insulin. Many people notice that even when their diet doesn’t change much, their blood sugar tends to run higher in the winter. This often comes down to a drop in insulin sensitivity. In simple terms, your cells don’t respond to insulin as efficiently in colder months, which means sugar stays in the bloodstream longer instead of being absorbed as energy. But why does this happen? One big reason is that the body goes into a kind of “preservation mode.” The cold naturally increases stress hormones, which interfere with insulin’s ability to do its job properly.
Another contributing factor is reduced physical activity. When temperatures drop, most people naturally move less. They skip outdoor walks, avoid exercise due to cold air, and spend more time relaxing indoors. Less movement means muscles aren’t using glucose for fuel, which leads to higher blood sugar throughout the day. It’s like fuel sitting in a car’s tank without the car ever being driven—nothing is being burned, so everything just stays there. During the summer, people tend to stay more active without even thinking about it, so insulin sensitivity naturally improves.
Cold weather also influences eating habits, which indirectly affects insulin response. Heavier foods high in carbohydrates, sugar, and unhealthy fats are more common during winter. These foods take longer for the body to process, and the slower digestion rate paired with decreased insulin sensitivity creates the perfect combination for glucose spikes. The body simply struggles to manage the extra workload, especially when digestion slows in response to cold conditions.
Understanding how cold weather affects insulin sensitivity gives you the power to adjust your routine wisely. Simple things like increasing indoor activity, choosing lighter meals, or drinking warm herbal teas that support glucose stability can significantly reduce winter blood sugar complications. Small, consistent actions have a big impact, especially when your body is working harder than usual to maintain balance during the colder months.
Winter Cravings and Carb-Heavy Comfort Foods
Winter cravings are no joke. The moment the air gets chilly, the body naturally starts wanting heavier, sweeter, and more comforting foods. Warm pastries, creamy soups, buttery breads, hot chocolate, and sugary holiday treats all start calling your name. But these cravings aren’t just about taste—they’re rooted in biology. When temperatures drop, the body burns more energy to stay warm, so it looks for quick fuel sources. Carbohydrates and sugary foods provide fast energy, which is why they suddenly feel irresistible in winter. Unfortunately, they are also the very foods that trigger rapid blood sugar spikes.
Another reason winter cravings intensify is due to hormonal changes. With less sunlight, the body produces more melatonin—the sleep hormone—and less serotonin, which is linked to mood and appetite regulation. Low serotonin levels can lead to cravings for “comfort foods” that temporarily boost mood. Add holiday gatherings, family celebrations, and stress eating into the mix, and you end up consuming far more carbs than your body can efficiently process, especially when you’re less active.
But managing these cravings doesn’t mean you have to give up all your favorite winter foods. The goal is to replace unhealthier options with smarter choices. For example, instead of sugary cocoa mixes, enjoy unsweetened hot cocoa with a natural sweetener. Swap creamy potato soups for hearty lentil soups packed with fiber and protein. Replace pastries with warm oatmeal topped with nuts and cinnamon. These options still give you the warm, cozy feeling you want, but without the blood sugar roller coaster.
It also helps to eat balanced meals throughout the day. When you skip meals or eat too little, your blood sugar drops and your body demands quick carbs to bring it back up. That’s when cravings hit the hardest. Eating enough protein, fiber, and healthy fats can reduce the desire for sugary foods dramatically. You can also try keeping healthy snacks around—like nuts, Greek yogurt, roasted chickpeas, or apple slices with peanut butter—to satisfy hunger without spiking glucose levels.
Learning how to manage winter cravings is not just about discipline; it’s about understanding what your body needs and giving it healthier ways to feel nourished and warm. When you strike that balance, cravings lose their power, and blood sugar stays steady even on the coldest days.
Importance of Hydration in Winter Blood Sugar Control

Most people associate dehydration with summer—sweating, heat, and thirst. But winter dehydration is even more common, and surprisingly, more dangerous for blood sugar control. Cold air is naturally drier, and as we breathe it in, the body loses moisture without us noticing. On top of that, indoor heating systems further dry the air, pulling moisture from your skin and lungs. Because you don’t feel as thirsty in winter, you simply don’t drink enough water. This is where trouble begins: when the body gets dehydrated, glucose becomes more concentrated in the bloodstream, causing blood sugar levels to rise.
Hydration plays a vital role in helping the kidneys flush out excess glucose. When you’re not drinking enough water, the kidneys struggle to balance sugar levels, leading to spikes that can linger for hours. Even people who maintain a clean diet and steady routine can see unexpected highs simply because they forgot to hydrate. If you’ve ever wondered why your numbers jump on cold mornings, dehydration is often the silent culprit.
Drinking more water is one of the easiest, most effective winter habits for controlling blood sugar—but it doesn’t always mean drinking plain cold water. In winter, warm fluids are far more comforting and easier to consume. Herbal teas, warm lemon water, hot infusions with mint or cinnamon, and broth-based soups all count toward hydration. These options not only keep you warm but also support digestion and metabolism, which naturally helps balance glucose levels. Cinnamon tea, for example, has been shown to support insulin sensitivity, making it a great winter-friendly drink.
Another tip is to eat hydrating foods. Fruits like oranges, apples, kiwi, and pears are not just packed with vitamins; they also contain natural water that helps replenish the body’s hydration. Winter vegetables like cucumbers, celery, leafy greens, and cabbage also contain water and fiber, making them excellent for glucose control. Hydrating through food is especially helpful for people who struggle to drink enough water during colder months.
Maintaining hydration throughout the day is key. A simple rule is to drink a glass of warm water after waking up, one before each meal, and one in the afternoon. This small routine keeps hydration steady and supports glucose stability. Once you’re aware of how dehydration affects blood sugar, staying hydrated becomes one of the easiest winter habits to integrate into your daily routine.
Maintaining Physical Activity During the Winter
When winter hits, motivation often takes a backseat. The chilly air, shorter days, and cozy blankets make it tempting to stay indoors and avoid any form of exercise. But here’s the truth: reduced physical activity is one of the biggest reasons blood sugar rises in winter. Movement helps cells absorb glucose more efficiently, improves insulin sensitivity, and keeps metabolism active. When activity levels drop, the body burns fewer calories, uses less glucose, and stores more sugar in the bloodstream. Even a few days of inactivity can noticeably impact blood sugar readings.
Winter also affects the way the body processes food. When you’re less active, digestion slows down, and insulin response becomes sluggish. Meals that wouldn’t cause much trouble in the summer can suddenly spike your sugar levels because your muscles aren’t using up that extra glucose. Add holiday meals, heavier foods, and increased stress, and you have a perfect mix for unstable numbers. This is why staying active—even just a little—becomes one of your strongest tools for controlling blood sugar during cold months.
The good news? You don’t need a gym membership or extreme workouts. Indoor activities work just as well. Walking around the house, climbing stairs, doing bodyweight exercises, or following YouTube workout videos can keep glucose levels stable. Even 10-minute movement sessions throughout the day can make a significant difference. Simple routines like jumping jacks, marching in place, or light stretching help keep the body warm, boost circulation, and activate muscles that support glucose use.
If you prefer a slow-paced activity, try yoga or indoor stretching flows. These gentle workouts reduce stress, improve flexibility, and enhance insulin sensitivity. Chair exercises are excellent for people with mobility issues or those who prefer low-impact routines. Dance workouts are another fun option—put on your favorite music and move for 15 minutes. Not only does it burn calories, but it also releases feel-good hormones that boost your mood during gloomy winter days.
Another helpful tip is to set movement reminders. Alarms or fitness apps can nudge you to get up and stretch every hour. Using a step counter also keeps you aware of how much you’re moving. Aim for small goals: 5,000 steps a day indoors is completely achievable. Even cleaning the house counts as physical activity—vacuuming, mopping, and organizing are all great ways to burn calories without feeling like you’re exercising.
The key is consistency. When you maintain some level of physical activity every day, your blood sugar remains far more stable, and your energy levels stay higher. Winter doesn’t have to be a season of inactivity—turn it into a season of steady, enjoyable movement, and your glucose levels will thank you.
Vitamin D and Its Role in Blood Sugar Regulation
Winter brings shorter days, cloudy skies, and limited exposure to sunlight—all of which contribute to a drop in vitamin D levels. What most people don’t realize is that vitamin D is not just a “bone health” nutrient; it plays a major role in insulin sensitivity and glucose metabolism. When vitamin D levels fall, the body struggles to regulate blood sugar effectively. This can lead to higher fasting glucose levels, more frequent spikes, and difficulty maintaining stable numbers throughout the day.
Low vitamin D affects the pancreas directly. The pancreas contains vitamin D receptors that help it produce and release insulin. When these receptors don’t receive enough vitamin D, insulin production becomes less efficient. At the same time, the body’s cells become less responsive to insulin, leading to insulin resistance. This creates a double challenge: the body produces less insulin, and the insulin it does produce doesn’t work as well. This is a major reason many people see their blood sugar unexpectedly rise during the winter months.
Another factor is that winter affects mood. Reduced sunlight can lead to seasonal mood changes and increased stress. Stress hormone levels—particularly cortisol—tend to rise when vitamin D is low. Cortisol directly raises blood sugar, making glucose management even harder. People may feel more tired, experience cravings, or struggle with low motivation—all of which contribute to less balanced eating habits. Fortunately, improving vitamin D levels can help stabilize mood, enhance energy, and reduce sugar cravings, making glucose control easier.
Getting enough vitamin D during winter doesn’t have to be complicated. Start with diet: include foods such as egg yolks, mushrooms, fortified cereals, fortified plant-based milks, fatty fish (like salmon), and yogurt. Spending even 10–15 minutes near a sunny window can help, though it won’t replace direct sunlight fully. If safe and appropriate, some people consider vitamin D supplements during winter months—but this should be done responsibly and ideally based on blood test results or medical guidance.
The key takeaway is that vitamin D is essential for glucose control, especially during winter. By paying attention to it, you support your body’s ability to regulate insulin, reduce resistance, and stay energized even on the cloudiest days. Addressing vitamin D deficiency becomes one of the most effective strategies for maintaining steady blood sugar levels all winter long.
Winter Stress Levels and Their Effect on Blood Sugar
Winter seems peaceful from the outside, but internally, it can be one of the most stressful seasons of the year. Cold weather, shorter days, increased responsibilities, and the pressure of holidays all contribute to a rise in stress levels. Stress may feel emotional, but its effect on blood sugar is very physical. When the body experiences stress—whether mild or intense—it releases cortisol, the primary stress hormone. Cortisol signals the liver to release stored glucose into the bloodstream to give you quick energy. This natural survival mechanism is useful in emergencies, but when stress becomes chronic, blood sugar remains elevated for long periods.
Holiday seasons often intensify stress. Family gatherings, financial planning, gift shopping, and busy schedules can trigger emotional overload. At the same time, people are eating richer meals, sleeping less, and moving less—all of which make stress-related glucose spikes even worse. Many people also turn to comfort foods when stressed, especially in winter. These foods are usually high in sugar and carbohydrates, which create a quick sense of relief before causing a big sugar crash later. Over time, the stress-eating cycle leads to unstable glucose levels and increased cravings.
Another overlooked factor is seasonal depression or “winter blues.” The lack of sunlight disrupts the production of serotonin and melatonin, affecting mood and sleep. When you’re feeling low, motivation drops and unhealthy habits take over—skipping meals, overeating, staying up late, or avoiding exercise. All of these habits feed directly into blood sugar instability. Stress and poor sleep together create a hormonal imbalance that increases insulin resistance, making it much harder to maintain stable glucose levels even with a healthy diet.
Managing winter stress doesn’t require drastic changes. Simple daily routines can make a significant difference. Start by practicing deep breathing for a few minutes each day. This relaxes the nervous system and helps lower cortisol levels. Gentle activities like stretching, yoga, or short walks—even indoors—release endorphins, which improve mood and help regulate glucose. Creating a calming nighttime routine also helps: dim the lights, avoid screens before bed, drink a warm herbal tea, and practice relaxation techniques that prepare the body for quality sleep.
Another helpful strategy is setting realistic boundaries during the holidays. It’s okay to say no to overwhelming commitments. Try to plan meals ahead of time, take short breaks throughout the day, and give yourself permission to rest without guilt. Keeping communication open with loved ones can also reduce emotional burden. When stress is managed, blood sugar naturally becomes more stable, proving that emotional well-being and physical health are deeply connected.
Healthy Winter Meal Planning for Blood Sugar Control
Meal planning in the winter can feel challenging because cravings change, routines shift, and warm, heavy foods become more appealing. However, with the right strategy, winter meals can be both satisfying and blood-sugar-friendly. The key is balance—balancing carbs with protein, fiber, and healthy fats to ensure a slow and steady release of glucose. When meals are balanced, you stay full longer, cravings decrease, and the body handles glucose more efficiently, even when activity levels drop.
One of the smartest winter meal-planning strategies is to focus on whole, unprocessed ingredients. Winter is a great season for nutrient-dense vegetables like cauliflower, kale, spinach, Brussels sprouts, cabbage, sweet potatoes, and carrots. These veggies are rich in fiber, vitamins, and antioxidants, making them perfect for supporting digestion and stabilizing blood sugar. When cooked in soups, stews, or sautéed dishes, they add warmth and comfort while still being healthy.
Protein should be the foundation of every winter meal. Whether you prefer chicken, turkey, eggs, tofu, beans, fish, or lentils, having a solid portion of protein slows carbohydrate absorption and prevents glucose spikes. Pairing protein with high-fiber sides—like quinoa, brown rice, barley, or whole grains—keeps meals satisfying. For people who enjoy traditional winter comfort foods, small modifications can make a big difference. For example, replace creamy pasta sauces with tomato-based ones, choose baked over fried dishes, or use whole-grain alternatives instead of white flour options.
Healthy fats are another important component. Adding avocado, nuts, seeds, or olive oil to meals helps maintain satiety and improves the body’s ability to process glucose. These fats don’t raise blood sugar and provide steady energy—perfect for cold days when your body needs extra warmth. Soups and stews are especially helpful in winter because they combine hydration, fiber, and nutrients in one comforting bowl. Just be mindful of creamy bases or high-carb additions like noodles or potatoes.
Snacks also matter in winter meal planning. Instead of sugary treats, choose high-protein and high-fiber options such as Greek yogurt, mixed nuts, roasted chickpeas, hummus with veggies, or fruit with nut butter. Preparing snacks ahead of time ensures you don’t reach for unhealthy options when cravings hit. Planning your meals weekly can also reduce stress and help you stay consistent. You save time, avoid impulsive eating, and maintain stable blood sugar even during the busiest winter days.
When you’re intentional about winter meals, food becomes a powerful tool for nourishing your body and supporting stable glucose. With balanced choices and comforting recipes, winter can be delicious, cozy, and blood-sugar-friendly—all at the same time.
Best Winter Foods That Help Stabilize Blood Sugar
Winter is the perfect season to enjoy warm, nourishing foods that support stable blood sugar. While many winter comfort meals can lead to glucose spikes, there are plenty of seasonal ingredients that naturally help regulate insulin, improve digestion, and maintain steady energy levels. The secret lies in choosing whole foods rich in fiber, protein, antioxidants, and slow-digesting carbohydrates. These foods keep you satisfied longer, reduce cravings, and provide steady nourishment during chilly days.
One of the most powerful winter-friendly blood sugar foods is leafy greens. Vegetables like spinach, kale, mustard greens, and Swiss chard are abundant during the colder months. They are low in carbohydrates and high in magnesium, a mineral that helps improve insulin sensitivity. Leafy greens also contain antioxidants that reduce inflammation—another contributor to unstable glucose levels. Adding them to soups, omelets, sautéed dishes, or smoothies is an easy way to increase nutrient intake.
Root vegetables, such as carrots, beets, turnips, and sweet potatoes, are also excellent choices when eaten in moderation. Although they contain natural sugars, their high fiber content ensures slow digestion and gradual glucose release. Roast them with olive oil, herbs, and spices for a warm, satisfying winter meal. Sweet potatoes, in particular, are rich in beta-carotene and potassium, making them more diabetic-friendly than regular potatoes when portioned properly.
Winter squashes, like butternut squash and pumpkin, are another great addition. They are loaded with vitamin A, fiber, and antioxidants. Enjoy them in soups, roasted side dishes, or purees without adding sugar. Their natural sweetness satisfies cravings without creating sudden glucose spikes.
Protein remains crucial for stable blood sugar, and winter provides many delicious, warming options. Lentils and beans, such as chickpeas, black beans, and kidney beans, offer a perfect blend of protein and fiber. They keep you full, support gut health, and prevent rapid glucose increases. Add them to stews, curries, or salads for hearty winter meals.
Spices also play a powerful role in winter blood sugar control. Cinnamon, for example, helps improve insulin sensitivity and reduces fasting glucose levels. Ginger supports digestion and reduces inflammation. Turmeric contains curcumin, a natural compound known to support metabolic health. Adding these spices to teas, soups, or roasted veggies enhances flavor while supporting glucose balance.
Don’t forget healthy fats—nuts, seeds, avocado, and olive oil help slow digestion and keep blood sugar steady. A handful of almonds or walnuts makes a perfect winter snack that satisfies hunger without raising glucose.
When combined thoughtfully, these winter foods create meals that are warming, delicious, and naturally supportive of balanced blood sugar. They nourish the body from the inside out and make winter healthier and more enjoyable.
Managing Morning Sugar Levels in Winter
Many people notice that their morning blood sugar levels are higher during winter—even before they eat breakfast. This can feel confusing, but it’s actually a result of several seasonal factors working together. The body naturally experiences the dawn phenomenon, a hormonal surge early in the morning that releases glucose to prepare you for the day. In winter, this effect intensifies because shorter daylight hours disrupt your circadian rhythm, leading to higher cortisol levels. Cortisol raises blood sugar, so mornings become a tricky time for glucose control.
Cold temperatures also contribute. When the body wakes up in a chilly environment, it releases more stress hormones to keep you warm. This causes the liver to dump glucose into the bloodstream, which elevates fasting blood sugar even more. Sleeping under heavy blankets or in overheated rooms can also interfere with sleep quality, which is directly linked to insulin sensitivity. Poor sleep combined with cold-weather hormonal changes makes morning sugar harder to manage.
A winter morning routine can make a huge difference. Start by drinking a warm glass of water as soon as you wake up. This helps rehydrate the body, activates digestion, and signals your metabolism to kick in. Hydration alone can lower fasting glucose levels. After that, try light movement—simple stretches, a short indoor walk, or a few minutes of yoga. Physical activity first thing in the morning encourages muscles to absorb glucose and helps regulate insulin response for the rest of the day.
Breakfast is another important part of morning sugar control in winter. Avoid high-carb breakfasts like pastries, sugary cereals, and white bread—they spike blood sugar rapidly. Instead, choose a protein-rich meal such as eggs, Greek yogurt, tofu scramble, chia pudding, or a vegetable omelet. Pairing protein with healthy fats and fiber keeps glucose levels stable. Adding cinnamon to your morning drink or oatmeal may also help, as it supports insulin function.
Keeping your sleep routine consistent is another effective strategy. Try to sleep and wake at the same time every day, even on weekends. This stabilizes hormone release and reduces the impact of dawn phenomenon. Additionally, aim for a bedroom temperature that is cool but not cold—cold rooms increase glucose-releasing hormones, while overly warm rooms disrupt sleep quality.
Finally, avoid checking your blood sugar immediately upon waking if possible. Levels naturally fluctuate, and checking 20–30 minutes later—after walking, stretching, or hydrating—often gives a more accurate picture. With the right winter morning habits, fasting glucose levels become far more predictable and easier to manage.
Sleep Patterns and Blood Sugar Control During Winter
Winter has a way of completely disrupting natural sleep rhythms. The shorter days, longer nights, and colder temperatures change how the body produces melatonin—the hormone responsible for sleep. When melatonin levels rise earlier in the evening, you may feel sleepy sooner than usual. But inconsistent sleep schedules, late-night screen time, and stress can interfere with this natural rhythm, causing irregular sleep patterns. Poor sleep is directly linked to insulin resistance, which means even one or two nights of disturbed rest can make blood sugar harder to manage.
Another winter-specific issue is oversleeping. While it may seem harmless, sleeping too long can throw off cortisol levels. Cortisol helps the body wake up, but when its timing becomes irregular, morning glucose spikes become more pronounced. Oversleeping also reduces morning physical activity, which means glucose stays elevated longer. On the other hand, sleeping too little increases hunger hormones like ghrelin and decreases leptin—the hormone that signals fullness. This leads to cravings, overeating, and unstable glucose throughout the day.
Cold bedrooms create another obstacle. When the body feels cold, it works harder to stay warm, increasing stress hormones and causing sleep interruptions. People often wake up feeling tired, even after a full night of rest. Inconsistent sleep quality leads to higher fasting sugar levels, increased insulin resistance, and more difficulty maintaining stable glucose in winter.
Improving winter sleep doesn’t require major lifestyle changes. Start by maintaining a consistent bedtime and wake-up time, even on weekends. This trains your internal clock and regulates hormone release. Keep your bedroom cool but not uncomfortably cold—ideally between 60–67°F (15–19°C). Use warm blankets instead of overheating the room, which can disrupt sleep cycles. Reducing screen exposure at least one hour before bedtime also helps, since blue light suppresses melatonin and delays sleep onset.
Lighter evening meals support better sleep as well. Eating heavy, high-carb dinners close to bedtime increases nighttime glucose spikes and disrupts restful sleep. Choose balanced dinners with protein, vegetables, and healthy fats. Warm herbal teas like chamomile, ginger, or peppermint can also calm the nervous system and prepare the body for deeper sleep.
Finally, consider creating a relaxing nighttime routine—dimmed lights, gentle stretching, deep breathing, or reading. These habits lower stress hormones and signal the body that it’s time to rest. With better-quality sleep, blood sugar becomes easier to manage, cravings decrease, and energy levels remain steady throughout the winter season.
How to Control Nighttime Sugar Fluctuations in Winter
Nighttime blood sugar can be especially unpredictable in winter. Many people notice their levels rising late in the evening or dropping unexpectedly while they sleep. This happens because winter alters the way the body processes energy at night. Colder temperatures increase the release of stress hormones as the body tries to stay warm, and these hormones push glucose into the bloodstream. At the same time, heavier winter dinners and holiday eating habits contribute to glucose spikes that can linger for hours. When you combine all this with disrupted sleep patterns, nighttime sugar levels become harder to predict and control.
One common cause of nighttime spikes in winter is eating large dinners. Comfort meals like creamy pasta, rice dishes, potatoes, and sweets are tempting on cold nights but cause glucose to rise slowly and stay elevated long after you’ve gone to bed. Because less physical activity happens after dinner in winter, the body has a harder time using up that extra glucose. The result: high readings before sleep or elevated fasting sugar in the morning.
Nighttime lows also occur more frequently in winter, especially if you eat dinner too early, restrict carbs too much, or increase insulin or medication without adjusting for seasonal changes. Cold weather increases calorie burning, so the body may use more glucose while you’re asleep, leading to sudden drops. This can trigger the liver to release stored sugar, causing a rebound high—a roller-coaster effect that feels confusing when you check your glucose in the morning.
A simple winter nighttime routine can bring balance back. Start by choosing lighter dinners rich in protein, fiber, and healthy fats. Examples include grilled vegetables with chicken, lentil soup, stir-fried tofu, or salmon with a side of broccoli. These meals are warm, comforting, and blood-sugar-friendly. Avoid eating 2–3 hours before bedtime to give your body time to process your meal.
Incorporating a short walk after dinner—even 10 minutes indoors—can make a dramatic difference. Movement helps muscles absorb glucose, reducing the chance of nighttime spikes. If walking isn’t possible, gentle stretching or slow-paced yoga also helps regulate blood sugar and relax the body for sleep.
Warm drinks like cinnamon tea or chamomile can support stable glucose levels before bed. However, avoid hot chocolate, sweetened beverages, and heavy snacks late at night, as they cause delayed glucose rises.
Finally, keep your bedroom comfortably warm. Sleeping in a very cold room increases stress hormones, while an overly hot room disrupts sleep cycles—both of which impact glucose. Aim for a cozy balance.
With the right nighttime habits, winter will no longer cause unpredictable sugar swings, and you can wake up with stable, steady levels.
Safe Winter Snacking for Blood Sugar Management
Winter snacking can be one of the biggest challenges for keeping blood sugar stable. Cold weather naturally increases appetite, making you crave warm, comforting foods throughout the day. Unfortunately, most common winter snacks—cookies, pastries, chips, hot cocoa, holiday treats—are loaded with sugar and refined carbs that spike glucose quickly and crash it just as fast. This leads to hunger, fatigue, irritability, and unstable blood sugar patterns that continue for hours. The key to winter snacking is choosing foods that are warm, satisfying, and rich in nutrients without causing glucose spikes.
A smart winter snack should include a combination of protein, fiber, and healthy fats. These nutrients slow digestion, keep you full longer, and ensure steady energy. For example, a handful of almonds or walnuts offers warmth, crunch, and steady fuel. Nuts also contain magnesium, which supports insulin sensitivity. Pairing fruit like an apple or pear with a tablespoon of peanut butter creates a balanced snack that satisfies cravings without spiking sugar.
Warm snacks are especially comforting in winter. Consider making a cup of unsweetened herbal tea with a small handful of mixed seeds. Pumpkin seeds and sunflower seeds are excellent because they contain zinc and healthy fats that regulate blood sugar. A bowl of warm oatmeal with cinnamon, chia seeds, and a few berries is another great option—fiber-rich, cozy, and glucose-friendly when not overloaded with sweeteners.
If you prefer savory snacks, roasted chickpeas, boiled eggs, or vegetable soups are perfect winter choices. These fill you up without overwhelming your system with carbohydrates. A small plate of hummus with cucumber and carrot sticks is another satisfying option that delivers protein and fiber together. Even popcorn can be a healthy winter snack if air-popped and lightly seasoned—just avoid the buttery or sugary varieties.
The biggest trap during winter is mindless snacking. Staying indoors more often, watching TV, or working from home can lead to unconscious eating. To avoid this, plan your snacks ahead of time. Preparing snack containers for the week ensures you always have healthy options ready. Another helpful strategy is drinking warm beverages between snacks. Sometimes what feels like hunger is actually dehydration—very common in winter. Warm lemon water, cinnamon tea, ginger tea, or mint tea can reduce cravings and hydrate your body.
The best winter snacking habit is listening to your body. Eat when you’re truly hungry, choose nourishing foods, and enjoy snacks that keep you energized and satisfied. When snacking becomes intentional, winter becomes much easier to manage—both emotionally and metabolically.
Winter Supplements That Support Blood Sugar Control
Winter is a season when many people naturally become deficient in essential nutrients that help regulate blood sugar. Reduced sunlight, lower activity levels, changes in appetite, and heavier meals all place extra stress on the body’s glucose management systems. While food should always be the foundation of good health, certain supplements can offer additional support during winter—especially when used wisely and consistently. These supplements do not replace a balanced diet, but they can make controlling blood sugar easier when your body is under seasonal strain.
One of the most valuable winter supplements is vitamin D. With shorter days and limited sun exposure, vitamin D levels drop significantly. Low vitamin D is linked to insulin resistance, poor glucose control, fatigue, increased cravings, and weakened immunity. A deficiency can make blood sugar swing more dramatically. Including vitamin D-rich foods helps, but many people need extra support during colder months, especially if they spend most of their time indoors.
Another powerful supplement is cinnamon extract. Cinnamon has natural compounds that mimic insulin, helping the body process glucose more efficiently. Studies suggest that cinnamon can lower fasting glucose and improve overall insulin sensitivity. Adding cinnamon to foods is helpful, but supplements offer a more concentrated and predictable way to gain its benefits—especially during winter when carb-heavy meals are more common.
Magnesium is also critical for blood sugar control. It plays a role in more than 300 enzymatic processes in the body, including those responsible for glucose metabolism. Low magnesium levels are associated with higher blood sugar, increased insulin resistance, muscle cramps, and poor sleep—all issues that tend to worsen during winter. Foods like nuts, seeds, leafy greens, and beans contain magnesium, but many people still fall short, making supplementation beneficial.
Omega-3 fatty acids are another helpful option. These healthy fats reduce inflammation—a major contributor to insulin resistance. Winter diets often lack fresh produce and lean proteins, which makes inflammation more likely. Omega-3s help keep cells flexible, improve heart health, and support more stable glucose levels. They also help reduce winter mood swings, which can influence eating habits and cravings.
For digestive support, probiotics can be extremely valuable. Winter meals are often heavier and richer, slowing digestion and causing bloating or discomfort. Poor gut health is directly linked to unstable blood sugar because the gut influences everything from nutrient absorption to hormone balance. A good probiotic can help stabilize digestion, reduce inflammation, and support more predictable glucose patterns.
Chromium is another supplement that helps improve how the body processes carbs. It enhances insulin’s effectiveness and promotes steady glucose uptake by the cells. Chromium-rich foods like eggs, broccoli, and nuts are helpful, but during winter—when diets shift—supplementation can keep levels stable.
It’s important to remember that supplements work best when paired with healthy habits. Balanced meals, hydration, movement, and quality sleep are the foundation. Supplements enhance these efforts by filling nutritional gaps created by winter lifestyle changes. With consistent use, they can make blood sugar management smoother and more predictable, even when the cold weather challenges your routine.
Long-Term Winter Strategy for Consistent Blood Sugar Control
Managing blood sugar during winter isn’t just about making a few healthy choices here and there—it’s about developing a long-term strategy that carries you smoothly through the entire season. Winter brings a unique combination of challenges: colder temperatures, reduced daylight, increased cravings, heavier meals, lower motivation, and disrupted routines. Without a clear plan, it becomes easy to fall into habits that push blood sugar higher. But with a smart, sustainable strategy, winter can become one of the easiest seasons for glucose control rather than the hardest.
The first step in creating a long-term winter strategy is consistency. Your body thrives on predictable patterns. Even if your meals change slightly from day to day, maintaining regular meal times helps stabilize insulin response. Eating breakfast, lunch, and dinner around the same time prevents the dramatic highs and lows that occur when the body becomes confused about when to expect fuel. Winter can make you feel sleepier or hungrier at odd hours, but sticking to a routine supports balance.
Another important element is meal planning in advance. When you prepare weekly menus or batch-cook meals, you eliminate the temptation to resort to unhealthy comfort foods. Soup jars, roasted vegetables, protein-rich dishes, and pre-portioned snacks can be prepared ahead of time. This approach reduces stress, saves time, and makes it easier to choose nourishing foods even on cold, busy days. Planning also keeps your grocery shopping focused, avoiding sugary treats and snacks that sneak their way into the house during winter.
Physical activity is one of the pillars of long-term winter blood sugar control. Even light movement—like indoor walking, stretching, or bodyweight exercises—does wonders for insulin sensitivity. The trick is to make it enjoyable. If you love music, dance for 10 minutes. If you enjoy calm routines, try yoga. If you want something simple, set a timer and walk inside your home. Building movement into your everyday schedule ensures that your metabolism stays active, even when the cold weather tempts you to stay still.
Monitoring your blood sugar more regularly in winter is another smart strategy. Because the body reacts differently to cold weather, tracking patterns helps you understand your personal triggers. Some people see higher fasting numbers, while others notice spikes after dinner or during stressful holiday weeks. Keeping notes or using an app can help you make quick adjustments—like changing meal timing, increasing hydration, or adjusting portion sizes.
Managing stress is equally essential. Winter brings emotional challenges, especially during the holiday season. Practicing breathing exercises, journaling, connecting with loved ones, and taking regular breaks prevents stress-related spikes. A calm mind supports stable glucose.
Finally, make sure to support your body with hydration, vitamin D, and adequate sleep. These three factors are easily overlooked, yet they play massive roles in winter blood sugar stability. When they are aligned, your glucose levels respond beautifully.
Winter becomes much easier to manage when you approach it with a clear, practical strategy. Instead of reacting to challenges daily, you build habits that carry you through the season with confidence and control.
Conclusion
Controlling blood sugar during winter may feel challenging, but it becomes manageable—and even empowering—when you understand what your body is experiencing. From the impacts of cold weather on insulin sensitivity to winter cravings, dehydration, stress, sleep disruptions, and comfort eating, every factor plays a role in glucose stability. By making small, consistent adjustments—like staying hydrated, choosing balanced meals, staying active indoors, supporting nutrient levels, and creating a calming routine—you can maintain steady blood sugar all season long.
Winter doesn’t have to be a season of struggle. It can become a time of nourishment, warmth, and healthier habits. With awareness, preparation, and consistency, your body can thrive even on the coldest days. Use these strategies to support your health, stay energized, and enjoy the winter months with confidence and balance.
FAQs
- Why does blood sugar increase in winter even if I eat normally?
Cold weather raises stress hormones, reduces insulin sensitivity, and decreases activity levels—all of which contribute to higher glucose. - Do winter cravings affect blood sugar control?
Yes. Craving carb-heavy comfort foods is common in winter, but these foods can lead to rapid glucose spikes if not balanced with protein and fiber. - Is dehydration really an issue in cold weather?
Absolutely. Winter air is dry, and people feel less thirsty. Dehydration makes glucose more concentrated in the bloodstream. - How can I stay active indoors during winter?
Light home workouts, walking inside, yoga, and stretching are all effective. Even 10–15 minutes a day improves insulin sensitivity. - Are supplements necessary during winter?
Not mandatory, but supplements like vitamin D, magnesium, omega-3, and probiotics can support blood sugar control when winter conditions cause deficiencies.


Leave a Reply