Missing your period can spark a mix of emotions—excitement, anxiety, confusion, or even fear—depending on your life situation. But whether you’re hoping for a positive test or praying for a negative one, there’s always the same burning question: When should you actually take a pregnancy test for the most accurate result? Many people rush to take a test too early, which often leads to false negatives, unnecessary stress, and repeated testing. That’s why doctors recommend understanding your cycle, your symptoms, and the science behind how pregnancy tests work before peeing on that stick.
In this complete, human-style guide, we’ll walk through everything you need to know—why your period might be late, when doctors say it’s the right time to take a pregnancy test, what symptoms matter, which testing method is most accurate, and when a missed period might have nothing to do with pregnancy at all. The goal is simple: help you make sense of your body and give you clear, medically backed guidance so you don’t waste tests, time, or emotional energy.
We’ll break the topic into easy-to-understand sections, mixing medical facts with relatable examples—because let’s face it, your menstrual cycle doesn’t always behave like it’s supposed to. Grab a cup of tea, take a breath, and let’s figure out what your missed period is trying to tell you.
Understanding the Early Signs of Pregnancy

Early pregnancy often feels like PMS pretending to be something else. The symptoms overlap so much that most people have trouble telling the difference. But understanding these early clues can help you decide when to take a pregnancy test instead of testing randomly and getting unreliable results.
For many women, the first noticeable sign is breast tenderness—but this is also one of the most common premenstrual symptoms. Hormones like estrogen and progesterone surge right after conception, and they can make your breasts feel fuller, heavier, or sore. Then there’s fatigue, a symptom people often underestimate. Early pregnancy fatigue can hit like a truck; even a full night’s sleep can leave you exhausted. The reason? Your body is rapidly increasing blood production, supporting the uterine lining, and adjusting to rising hormone levels.
Another big sign is nausea, often called morning sickness, though it can strike at any hour. It’s caused by hCG, the hormone pregnancy tests look for. For some, it appears as early as 10 days after conception. For others, nausea never happens at all—so you can’t rely on it as a sure sign.
You might also notice light spotting, known as implantation bleeding. This light pink or brown spotting happens when the fertilized egg attaches to the uterine wall—typically 6–12 days after ovulation. The trouble is, many people mistake this for an early, light period. That’s why timing matters so much.
Other early pregnancy symptoms include:
- Increased urination
- Mild cramping
- Mood swings
- Food cravings or aversions
- Heightened sense of smell
But here’s the part most people overlook:
You can have several symptoms and still not be pregnant—and you can have almost no symptoms and get a positive test.
That’s exactly why doctors recommend focusing less on symptoms and more on the timing of your cycle when deciding when to test.
What Happens in Your Body After Conception
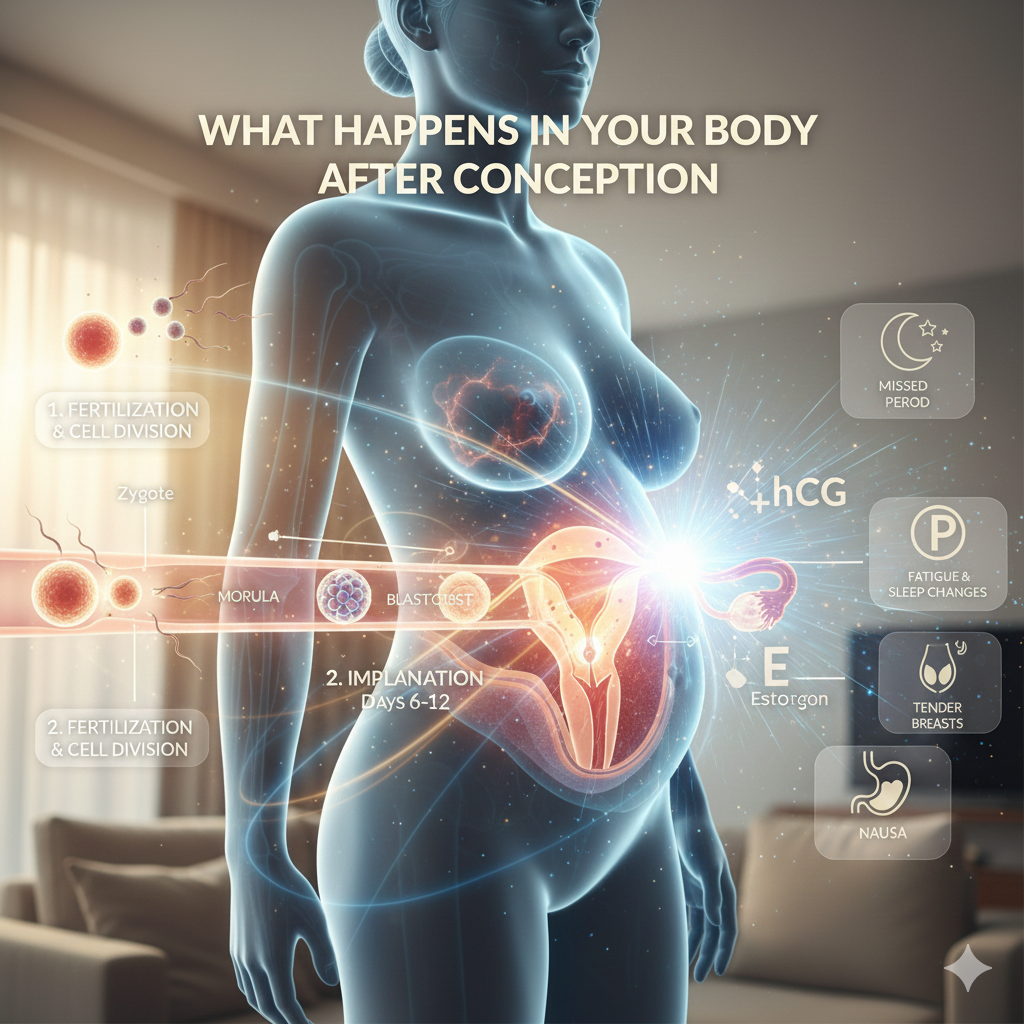
Once conception occurs, your body begins a series of rapid, intricate changes that prepare it to support a pregnancy. Many people don’t realize that these changes start long before you experience any noticeable symptoms. In fact, the earliest signs of pregnancy happen at a cellular level.
After an egg is fertilized, it begins dividing into multiple cells as it travels through the fallopian tube. This journey takes about 3–5 days. Once it reaches the uterus, the developing embryo starts searching for a place to attach—this is when implantation occurs. Implantation typically happens between 6 and 12 days after ovulation, and it marks the true beginning of pregnancy in a medical sense. This is also the moment your body begins producing hCG, the hormone detected by pregnancy tests.
The hormone hCG (human chorionic gonadotropin) rises quickly—doubling approximately every 48 to 72 hours in a healthy early pregnancy. This hormone signals the body to stop shedding the uterine lining, which is why your period doesn’t show up. It also supports the corpus luteum, a temporary gland that produces progesterone to maintain the uterine lining for the developing embryo. Rising progesterone levels are responsible for many early pregnancy symptoms: breast soreness, bloating, fatigue, and even mood changes.
Another major change is the increased blood flow. Your heart starts working harder, pumping more blood to deliver nutrients and oxygen to the embryo. This increase in blood volume is partly why some women feel more tired or lightheaded in early pregnancy.
Although all these changes are happening, it takes time before your hCG levels become high enough to be detected on a pregnancy test. That’s why testing too early—even if conception has occurred—often leads to a false negative. Doctors emphasize that your body is not a machine with predictable timers; implantation can happen later than expected, which means hCG will rise later too.
In short, your body begins to change the moment a fertilized egg implants, but the hormones need time to build up before any test can confirm pregnancy. Understanding this timeline is key to knowing when to test accurately.
When Doctors Recommend Taking a Pregnancy Test

One of the most common questions people ask is:
“How soon after missing my period should I take a pregnancy test?”
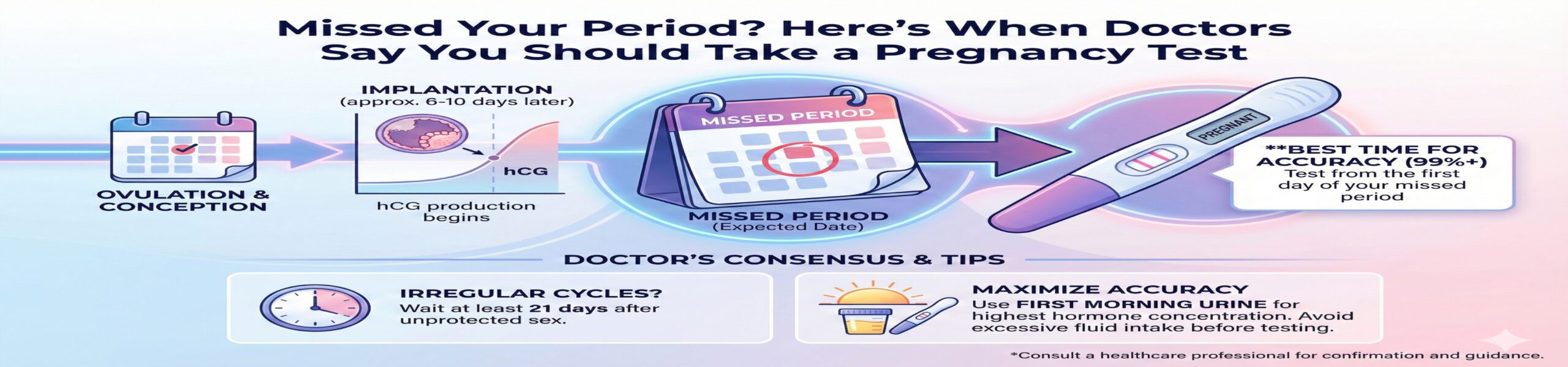
Doctors give a clear and consistent recommendation — test one week after your missed period for the most accurate results. This is because hCG levels vary widely from person to person, and even from pregnancy to pregnancy. Some people produce enough hCG early on to be detected right after their missed period, while others may not show up positive until several days later.
The typical menstrual cycle lasts about 28 days, with ovulation occurring around day 14. However, your body doesn’t follow a calendar—it follows biology. Ovulation may happen earlier or later, which affects when implantation occurs and when hCG begins to rise. If you ovulate late, for example, your hCG levels will rise later, making early testing unreliable.
Doctors generally recommend:
- If your cycle is regular: Test 7 days after your missed period.
- If your cycle is irregular: Wait at least 14 days after the date you believe ovulation occurred.
- If you had unprotected sex and don’t know your ovulation date: Test 21 days after intercourse for the highest accuracy.
There are certain situations when doctors say you should test earlier:
- You experience intense early pregnancy symptoms
- You have unexplained spotting
- You feel persistent nausea
- You have a history of irregular or unpredictable periods
- You’re actively trying to conceive and tracking ovulation
However, even in those cases, testing too early may cause unnecessary confusion. A negative test might simply mean you tested before your hCG levels reached a detectable threshold, not that you’re not pregnant.
Ultimately, doctors stress that timing is everything. A pregnancy test is only as accurate as the day you take it. Waiting that extra week might feel impossible, but it significantly increases your chances of getting a reliable answer the first time.
How Pregnancy Tests Work
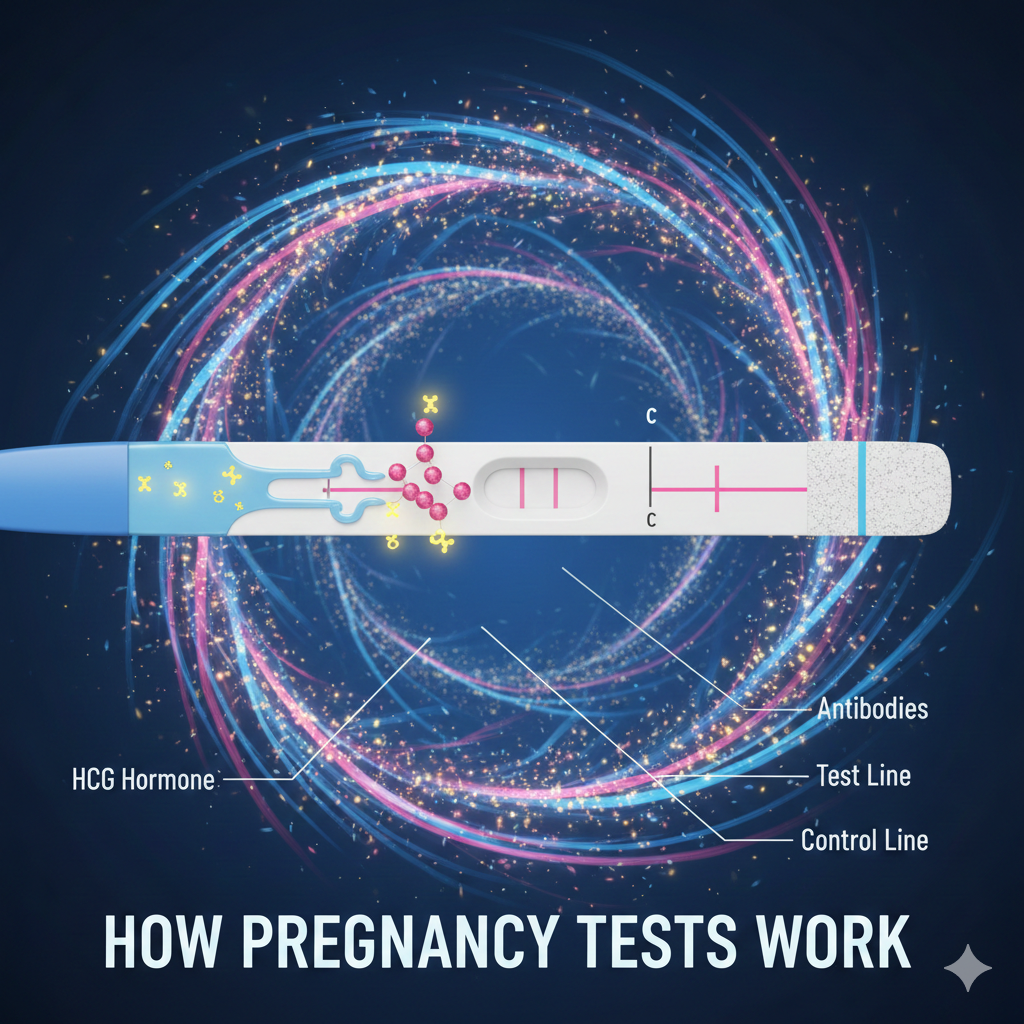
Pregnancy tests—whether done at home or in a medical setting—work by detecting hCG, the hormone your body produces during pregnancy. But how does that small stick you pee on actually know what’s happening inside your body? The science behind it is surprisingly simple yet incredibly precise.
Home pregnancy tests contain special antibodies that are designed to identify hCG in your urine. When your urine moves across the test strip, these antibodies bind to the hCG molecules. If enough hCG is present, the chemical reaction triggers a color change that forms the line you see on the test window. This line doesn’t measure how much hCG is present—it simply indicates whether the hormone has reached the threshold needed to cause the reaction.
Different tests have different sensitivity levels. Some detect very low hCG levels (as low as 10 mIU/mL), while others require higher amounts (around 20–25 mIU/mL). More sensitive tests can detect pregnancy earlier, but they also come with a higher chance of false negatives if the hormone hasn’t risen consistently yet.
There are two main types of pregnancy tests:
- Urine Pregnancy Test (Home test or in-office test)
- Convenient
- Non-invasive
- Detects hCG in urine
- Best used after a missed period
- Blood Pregnancy Test (Done by a doctor)
- Detects smaller amounts of hCG
- Can confirm pregnancy earlier
- Useful when monitoring early pregnancy issues
- Provides exact hCG levels
Blood tests come in two forms:
- Qualitative test: Gives a simple “yes or no” answer
- Quantitative test (beta hCG): Measures exact hormone levels
The accuracy of any pregnancy test—blood or urine—depends largely on when it’s taken. Even the most sensitive test won’t detect pregnancy before implantation, because hCG isn’t present until then. This is why doctors emphasize waiting until after your missed period or following the recommended timeline based on your cycle.
Understanding how these tests work helps you avoid misinterpreting results or testing prematurely.
Best Time of Day to Take a Pregnancy Test

Doctors consistently recommend taking a pregnancy test first thing in the morning, especially when testing early. The reason is simple: your urine is more concentrated after hours of not drinking water, which means it contains higher levels of hCG, the hormone pregnancy tests look for. When hCG is more concentrated, the chances of detecting pregnancy increase significantly.
In the early days of pregnancy, hCG levels are still relatively low. Testing with diluted urine—like after drinking several glasses of water—can cause the hormone to become too watered down to trigger a positive result. This is why many people get a negative test during the day but a positive result the next morning. It’s not magic; it’s just biology and concentration levels at play.
If you’ve already missed your period by several days or more, you’re more likely to get an accurate result at any time of the day. At that point, hCG levels are usually high enough that dilution doesn’t affect the test as much. However, if you want the strongest possible chance of accuracy—especially if it’s your first test—morning testing is still the best choice.
Here are a few helpful tips to follow:
- Use first-morning urine for the first test you take after a missed period.
- Avoid drinking excessive fluids before testing; this reduces the likelihood of dilution.
- Don’t test too late in the day if you’ve consumed a lot of water, soda, or tea.
- If your test is negative but you think you might be pregnant, retest the next morning for better accuracy.
- For those with an irregular cycle, morning testing is especially important, since you might not know exactly when implantation occurred.
Morning testing isn’t a strict rule—but it’s a medically backed strategy that significantly improves accuracy, especially in the early days after a missed period. It’s one of the simplest ways to reduce confusion, avoid false negatives, and get clearer answers without wasting multiple tests.
Most Accurate Pregnancy Test Timing According to Doctors

Timing is everything when it comes to pregnancy tests. No matter how sensitive a test claims to be, the most accurate results almost always come when you follow doctor-recommended timing. The general medical consensus is that the most reliable result occurs one week after your missed period, or at least 14 days after ovulation.
Why 14 days? Because pregnancy tests detect the hormone hCG, and this hormone only rises after implantation—which can happen anywhere from 6 to 12 days post-ovulation. If implantation occurs later than expected, your hCG levels may be too low to detect during early testing. This is why some people who ovulate late or implant late will consistently get negative tests even though they are pregnant.
Doctors often use the “14-day rule” because it covers all of the biological variation that can occur:
- Early implantation
- Late implantation
- Irregular ovulation
- Variations in hCG production
Even the most sensitive early-detection tests cannot override your body’s natural timeline. A test simply cannot detect pregnancy if hCG hasn’t reached a measurable threshold yet.
Here’s a breakdown of doctor-recommended timing:
- 3–4 days before period: Very unreliable
- On the day of your missed period: More reliable but still not perfect
- 3 days after missed period: Good chance of accuracy
- 7 days after missed period: Most accurate for almost everyone
- 14 days after possible conception: Ideal for irregular cycles
For people who don’t have predictable periods, doctors recommend waiting three weeks after intercourse. This timeframe accounts for late ovulation, late implantation, and individual differences in hCG levels.
In short, the best timing isn’t about impatience—it’s about biology. Waiting these extra days can spare you stress, reduce the number of tests you waste, and help ensure your results reflect what’s actually going on in your body.
Early Pregnancy Test vs. Standard Pregnancy Test

Many people wonder whether early pregnancy tests are truly worth it. Early detection tests are designed to identify lower levels of hCG, promising results even before your period is due. While they can be helpful, doctors caution that they aren’t always as accurate as standard tests taken after your missed period.
The main difference lies in sensitivity. Early tests can detect hCG levels as low as 10 mIU/mL, making them capable of identifying pregnancy earlier than standard tests, which typically require 20–25 mIU/mL. However, detecting lower levels of hCG also means early tests run a higher risk of false negatives if implantation hasn’t occurred yet or if your body produces hCG more slowly.
Standard pregnancy tests are considered more reliable because they’re designed to detect hCG levels that are typically present once a period is late. These tests have fewer false negatives and are less affected by natural variations in hormone levels.
Key differences:
- Sensitivity: Early tests detect low hCG; standard tests detect higher levels.
- Accuracy: Standard tests provide more consistent accuracy after a missed period.
- Timing: Early tests are best for “can’t-wait” situations, but still unreliable if taken too soon.
- False negatives: More common with early tests due to low hormone levels.
- Peace of mind: Standard tests reduce the emotional rollercoaster of uncertain early results.
Doctors emphasize that early tests can be useful, but they should always be followed up with a standard test after a missed period. This ensures you’re not misled by a result that doesn’t match your hormone timeline. Early tests are helpful tools, but they shouldn’t replace medically recommended timing.
Symptoms That Mean You Should Test Immediately

When you miss a period, it’s natural to wonder whether you should grab a pregnancy test right away or wait a few days. But beyond a missed period, there are certain symptoms doctors say should prompt immediate testing, because they strongly align with early pregnancy—even when your cycle is unpredictable.
One of the biggest signs is persistent nausea, especially if it’s paired with a heightened sense of smell. If simple everyday scents—like coffee, perfume, or food cooking—suddenly make your stomach churn, it may be time to test. Another strong sign is breast sensitivity that feels noticeably different from typical PMS. Pregnancy-related breast tenderness often feels deeper, heavier, or more swollen, and some people describe it as a warmth or fullness that wasn’t present during past cycles.
Another early symptom doctors highlight is increased urination, especially during the night. You might feel like you’re constantly running to the bathroom despite drinking the same amount of fluid as usual. This happens because rising hCG and progesterone levels increase blood flow through your kidneys, causing your body to produce more urine.
Then there’s unexplained fatigue—not the “I stayed up too late last night” kind, but the “I can barely keep my eyes open” kind. Early pregnancy fatigue is almost in a category of its own. This sudden crash of energy happens because your body is diverting energy toward building a placenta, supporting hormonal changes, and increasing blood production. If you feel drained for no clear reason, especially alongside other symptoms, a pregnancy test is warranted.
Some women experience implantation bleeding—light spotting that’s pink or brown. This is a key sign that can easily be mistaken for an early or light period. However, implantation bleeding is typically much lighter and shorter than a normal period. If you see spotting that isn’t quite like your usual cycle, testing early may be helpful.
Additionally, new food aversions or cravings, unexplained dizziness, or mood swings that seem more intense than usual may signal early pregnancy. These symptoms alone don’t guarantee pregnancy, but when two or more occur together—especially following a missed period—they’re strong indicators.
Doctors note that your intuition matters, too. If something feels “off” with your body and you suspect pregnancy, testing right away can provide clarity. Even if the test is negative, taking one gives you a starting point. If symptoms continue or intensify, retesting after a few days or following the recommended timing can help confirm what’s going on.
Understanding False Negatives
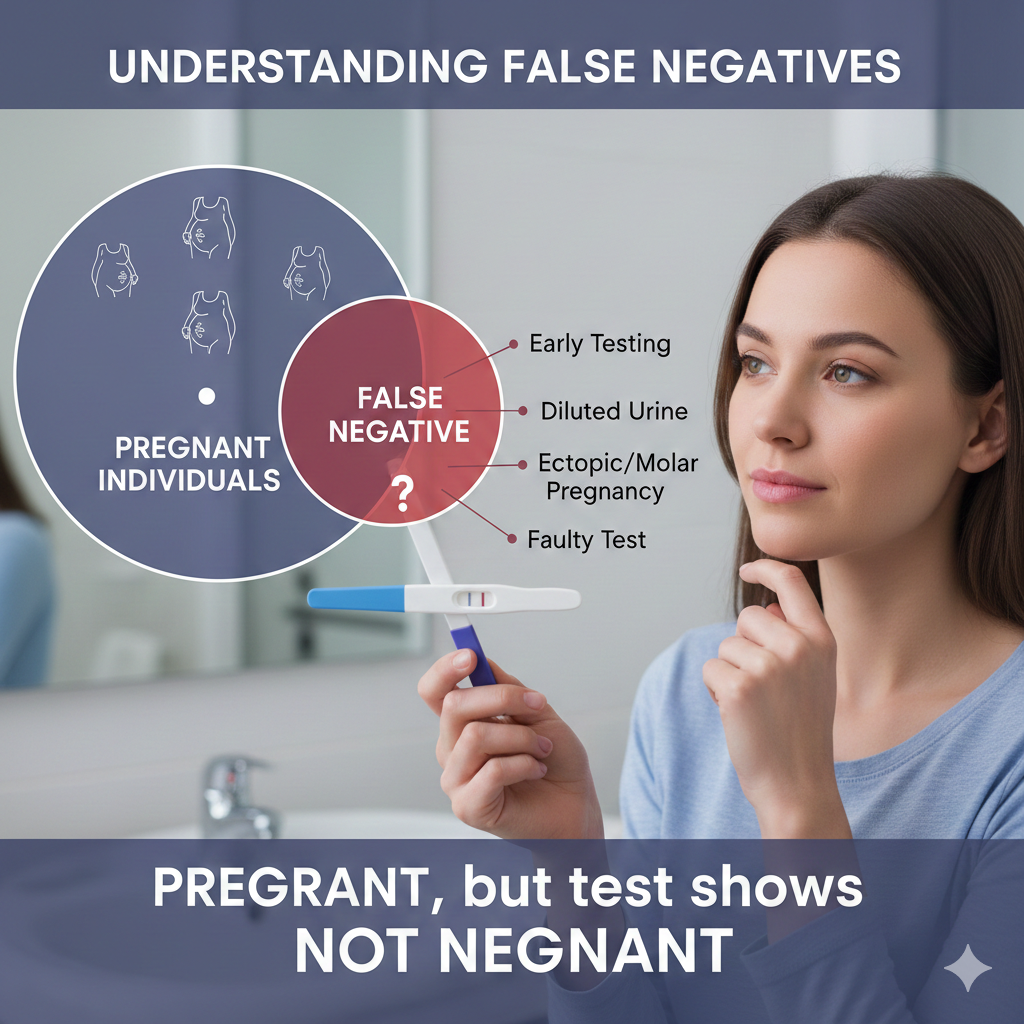
A false negative pregnancy test—when the test says “not pregnant” even though you are—can be incredibly stressful. It can leave you confused, anxious, and unsure of what your body is telling you. Doctors explain that false negatives happen more often than people think, especially when testing too early or not following proper instructions.
One of the most common reasons is testing before hCG levels are high enough to detect. Pregnancy tests look for a minimum threshold of hCG in urine, and if your body hasn’t reached that level yet, the test simply won’t pick it up. Implantation timing varies widely from woman to woman. If implantation happens late—say, 11 or 12 days after ovulation—you may not get a positive result until several days after your missed period.
Another reason for false negatives is diluted urine. Drinking a lot of water or fluids before testing can water down the concentration of hCG. This is why testing first thing in the morning is so important, especially in early pregnancy.
Sometimes, a false negative happens because the test wasn’t used correctly. Not following the timing directions, using an expired test, or checking the result too early or too late can lead to inaccurate results. Even something as simple as not holding the test in the urine stream long enough can impact the outcome.
A lesser-known cause of false negatives is the hook effect, where extremely high hCG levels oversaturate the test and produce a false negative. This is rare and usually occurs in later pregnancy or certain medical conditions, but it’s important to be aware that it can happen.
If you receive a negative test but still feel pregnant—or your period doesn’t arrive—doctors recommend retesting after 48 to 72 hours. Because hCG levels double every two to three days in early pregnancy, waiting a short period before retesting increases your chances of an accurate result.
False negatives can be confusing, but they’re not uncommon. Understanding why they happen makes it easier to interpret your results and decide when to test again.
Understanding False Positives

False positives—where the pregnancy test shows a positive result even though you’re not pregnant—are far less common than false negatives, but they do happen. When they do, they can be emotionally overwhelming, especially for those who are trying to conceive or for those who fear an unplanned pregnancy.
One of the most common causes of false positives is testing too soon after a miscarriage or chemical pregnancy. hCG levels remain in the body for days or even weeks after pregnancy ends, which means a test can still detect the hormone even though the pregnancy is no longer viable.
Another cause is evaporation lines—the faint gray lines that appear when a test dries. These lines aren’t truly positive results, but they can look like faint positives if you read the test after the recommended time window. This is why it’s crucial to read results only within the timeframe listed in the instructions.
Certain medical conditions can also cause false positives, such as ovarian cysts, hormonal imbalances, or rare disorders that cause elevated hCG levels. While these situations are uncommon, they highlight why a positive test should be followed up with a second test or a medical visit for confirmation.
Some medications—especially fertility treatments—can contain synthetic hCG, leading to temporary positive results. If you are undergoing fertility treatment, doctors recommend waiting the appropriate number of days after your final injection before taking a test to avoid misleading results.
Although false positives are rare, doctors advise confirming with two tests taken at least 24 hours apart. If both are positive, scheduling a medical appointment is the next step. A blood test or ultrasound can confirm whether a pregnancy is developing normally.
Understanding false positives helps reduce confusion and guides you toward the right next steps.
Blood Pregnancy Test: When It’s Needed
While home pregnancy tests are the first choice for most people, there are situations when doctors recommend getting a blood pregnancy test instead. Blood tests are more sensitive, more precise, and capable of detecting pregnancy earlier than urine tests. They also provide additional information that home tests simply cannot offer.
A blood pregnancy test comes in two main forms:
- Qualitative hCG test – tells you yes or no on pregnancy
- Quantitative beta hCG test – measures the exact amount of hCG in your bloodstream
Doctors typically recommend a blood test when the accuracy of a urine test is questionable, especially in early pregnancy. Blood tests can detect even tiny amounts of hCG—levels as low as 1 to 5 mIU/mL—making them useful for confirming pregnancy before a missed period or shortly after a faint positive on a home test.
Blood tests are also recommended if:
- You’ve had multiple negative urine tests but still have pregnancy symptoms
- You have irregular cycles and don’t know when ovulation occurred
- You think you got a false positive on a home test
- You’ve recently experienced a chemical pregnancy or miscarriage
- You’re undergoing fertility treatment
- Your doctor needs to track hCG levels over time to monitor a pregnancy
One major advantage of a quantitative test is its ability to measure how quickly hCG is rising. In a healthy early pregnancy, hCG should double approximately every 48–72 hours. If your levels are rising too slowly or not doubling at all, it may signal concerns such as ectopic pregnancy or early miscarriage. This is why doctors rely on blood tests when close monitoring is needed.
Another important reason for blood tests is suspected ectopic pregnancy, where a fertilized egg implants outside the uterus. Early symptoms may be mild or mistaken for regular pregnancy signs, but the risks are serious. Blood testing helps detect ectopic pregnancies earlier, allowing for prompt medical care.
In summary, blood pregnancy tests offer unmatched accuracy and insight, especially when a home test doesn’t give clear answers. If your results are confusing, inconsistent, or you feel something isn’t right, a blood test is the most reliable next step.
When a Missed Period May Not Mean Pregnancy
A missed period often triggers thoughts of pregnancy, but it’s important to remember that many other factors can influence your cycle. Doctors emphasize that missing a period does not automatically mean you’re pregnant. Your menstrual cycle is sensitive and can be affected by physical, emotional, and environmental changes.
One of the biggest reasons for a missed period is stress. High levels of stress can disrupt your hormonal balance, especially the hormones responsible for ovulation. When you don’t ovulate, you don’t get a period. This condition is called anovulation and is extremely common during times of emotional strain, major life changes, or chronic stress.
Weight fluctuations also play a major role. Significant weight loss, excessive dieting, or increased exercise can lower estrogen levels, leading to missed or irregular periods. On the other hand, rapid weight gain may also disrupt your cycle. Your body views extreme changes in weight as a signal that it’s not an ideal time for pregnancy, so it adjusts hormones accordingly.
Hormonal imbalances are another major cause of missed periods. Conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, or elevated prolactin levels can interfere with ovulation. For women with PCOS, irregular or missed periods are common, even when they’re not pregnant.
Birth control methods can also influence your cycle. Hormonal contraceptives may cause lighter periods, irregular periods, or even no periods at all. After stopping birth control, your body may take several months to adjust and return to its natural rhythm.
Other possible reasons for a missed period include:
- Recent illness
- Poor sleep
- Traveling or changing time zones
- Chronic medical conditions
- Perimenopause
In essence, your menstrual cycle is like a monthly report on how your body is doing. A missed period is a signal—but not always a pregnancy signal. That’s why doctors encourage looking at your overall health and lifestyle before jumping to conclusions. If you’ve missed a period but your pregnancy test is negative, it may simply be your body responding to stress or change. If your period remains absent for several cycles, a medical evaluation is recommended to identify the underlying cause.
Irregular Periods: When Should You Take a Pregnancy Test?
If your menstrual cycles are irregular, knowing when to take a pregnancy test can feel frustrating and confusing. Unlike those with predictable 28–30-day cycles, you may not know exactly when you ovulated or when your period is “officially” late. Doctors say that in these cases, timing your pregnancy test requires a different approach—one based on symptoms, sexual activity, and how your body typically behaves.
For irregular cycles, the most reliable method is to take a test three weeks after unprotected intercourse. This timeline accounts for late ovulation and late implantation, reducing the chances of a false negative. Because conception depends entirely on ovulation—not on the calendar—waiting three weeks ensures your hCG levels have had time to rise, no matter when ovulation occurred.
If you experience pregnancy symptoms such as nausea, breast tenderness, fatigue, or increased urination, doctors suggest testing sooner rather than later. Symptoms can provide clues when the calendar cannot. If you test negative but symptoms persist, retest every 3–5 days until you get a clear result.
Tracking your body’s signals can also help. Many women with irregular periods use signs such as changes in cervical mucus, basal body temperature, or mid-cycle cramping to estimate ovulation. If you suspect ovulation occurred, testing 14 days after that date increases the accuracy of your result.
If you have a condition like PCOS, thyroid imbalance, or adrenal issues, your cycles may vary widely. In these situations, it’s especially important to rely on symptoms, sexual activity timing, and follow-up testing rather than assuming a period will arrive at a specific time.
Doctors note that irregular cycles often make pregnancy detection more challenging, but not impossible. The key is to be patient, track your symptoms, and test at the right intervals. If you have irregular cycles and are frequently unsure about pregnancy, discussing long-term cycle tracking with a healthcare provider may help bring clarity and reduce stress.
How Soon to See a Doctor After a Positive Test

Seeing that positive pregnancy test can trigger a rush of emotions—joy, fear, excitement, disbelief, or a mix of everything at once. But after the initial shock settles, the next big question is: “When should I see a doctor?” Doctors recommend that most women schedule their first prenatal appointment around 6 to 8 weeks of pregnancy, measured from the first day of your last menstrual period.
Why this timing? Because by 6 weeks, a doctor can usually confirm the pregnancy through ultrasound, check for early fetal development, and rule out complications like ectopic pregnancy. Too early, and the ultrasound may not show much, which can cause unnecessary anxiety.
However, certain circumstances require seeing a doctor sooner, sometimes even immediately. If you have a history of miscarriage, ectopic pregnancy, or fertility issues, you should contact your doctor as soon as you get a positive test. Early monitoring can help track your hCG levels, ensure the pregnancy is developing normally, and detect potential problems before they become serious.
If you experience symptoms such as severe abdominal pain, shoulder pain, dizziness, heavy bleeding, or fainting, you should seek medical care right away. These could be signs of ectopic pregnancy, which requires urgent treatment.
For women with chronic conditions like diabetes, thyroid disorders, PCOS, hypertension, or autoimmune diseases, early prenatal care is crucial. Doctors may need to adjust medications or monitor symptoms more closely to support a healthy pregnancy.
If the pregnancy was unplanned, early medical care is equally important. A doctor can discuss your options, provide counseling, and ensure you make informed decisions based on accurate medical information.
Another reason to see a doctor early is to confirm your due date. If your cycles are irregular or you’re unsure when you ovulated, an early ultrasound can help determine how far along you are and set an accurate timeline for prenatal care.
In short, the best time to see a doctor after a positive test is generally between 6 and 8 weeks—but certain symptoms, medical conditions, or pregnancy histories make early appointments essential. Trust your instincts; if something doesn’t feel right, reach out to a healthcare provider sooner rather than later.
Tips for Getting the Most Accurate Pregnancy Test Results
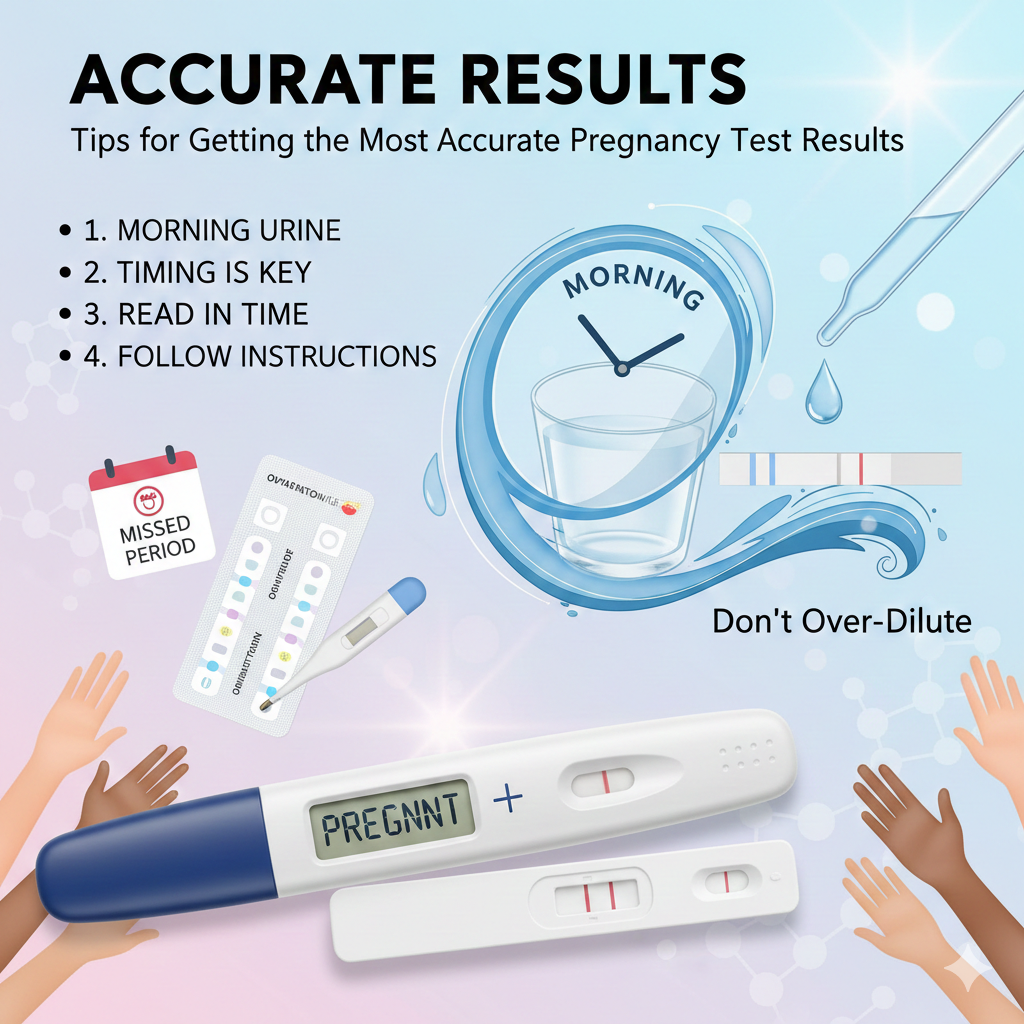
If you want the most reliable answer from a pregnancy test, timing isn’t the only thing that matters. How you take the test can influence the accuracy too. Many false negatives or confusing results happen because the test wasn’t taken under ideal conditions. Fortunately, a few simple tips can significantly boost your chances of getting a clear and accurate result the first time.
One of the most important tips is to use your first-morning urine, especially if you’re testing early. Morning urine is more concentrated, meaning hCG levels will be stronger and easier to detect. If you must test later in the day, try avoiding excess liquids for a few hours beforehand to prevent dilution.
Always read and follow the instructions carefully. It sounds obvious, but every test works slightly differently—some require holding it in a urine stream, while others need a urine sample in a cup. The timing window for reading the result also varies. Read too soon, and the test may not have finished processing. Read too late, and evaporation lines may appear, giving you a misleading impression of a positive result.
Check the expiration date as well. Expired tests may not work properly and can give inaccurate results. Store the test in a cool, dry place before use, as humidity and heat can affect the chemicals inside.
If your test result is unclear—such as a faint line—it’s best to wait 24 to 48 hours and test again. hCG levels double roughly every two days in early pregnancy, so a faint line one day may turn into a clear positive soon afterward.
If your period is late but you still get negative results, repeat testing every few days until your period arrives or until at least one week has passed. At that point, if tests are still negative, you may want a doctor consultation to explore other possible reasons for your missed period.
Ultimately, the most accurate result comes from combining proper timing, correct usage, and patience. Understanding how the tests work and giving your body time to show clear signs is key to avoiding false negatives and unnecessary stress.
When a Negative Test Still Requires Medical Attention
A negative pregnancy test usually brings clarity—either relief or disappointment—but sometimes, it raises new questions. What if you’re still missing your period? What if pregnancy symptoms persist? In these cases, a negative test doesn’t necessarily mean everything is normal. Doctors emphasize that certain situations require follow-up medical attention, even if the test says “not pregnant.”
One major reason to see a doctor after a negative test is continued absence of your period. If your period has been missing for more than six weeks, and you’re not pregnant, something else may be going on. Hormonal imbalances, thyroid issues, PCOS, pituitary gland disorders, and chronic stress can all disrupt your menstrual cycle. A doctor can run hormone tests and help identify the underlying cause.
If you’re experiencing strong pregnancy symptoms—nausea, fatigue, breast tenderness, or frequent urination—but your test remains negative, a blood test may be needed. Sometimes urine tests don’t detect very early pregnancy or fall short in cases of delayed implantation.
Another scenario that requires medical attention is severe pelvic pain, heavy bleeding, or dizziness. These symptoms could indicate ectopic pregnancy, which sometimes produces low hCG levels that home tests fail to detect. Ectopic pregnancy is a medical emergency, so any severe or unusual pain should be taken seriously.
If you’ve recently stopped or started birth control, or if you have a known reproductive condition, and your cycle seems off, a doctor can help monitor your body’s adjustment. Changes in medication, lifestyle, or health can all affect your cycle and may require medical guidance.
Finally, if you’ve been trying to conceive for over a year (or six months if over age 35) and are experiencing repeated negative tests, a doctor can help assess fertility factors on both sides.
A negative test usually ends the questions—but not always. If your symptoms don’t match the results, or your cycle is noticeably out of sync, reaching out to a healthcare provider is the best way to get clarity and peace of mind.
Conclusion
Missing your period can be nerve-racking, confusing, or exciting—sometimes all at once. But knowing when doctors recommend taking a pregnancy test can help you avoid wasted tests, unwanted stress, and inaccurate results. Whether your cycle is regular or unpredictable, the key is understanding how your body works, how pregnancy hormones rise, and why timing matters more than anything else.
A pregnancy test is only as accurate as the moment you take it. Testing too soon is the most common reason behind false negatives, while reading results incorrectly can lead to unnecessary panic. Waiting until one week after your missed period—or three weeks after intercourse if you have irregular cycles—gives you the clearest answer.
Pay attention to your symptoms, trust your body, and follow doctor-recommended guidelines for the most accurate results. And remember: a missed period doesn’t always mean pregnancy. Your cycle can be influenced by stress, lifestyle changes, hormones, and medical conditions. When in doubt, or if something feels off, seek medical advice. Your body deserves care, clarity, and attention.
FAQs
1. How long after missing my period should I take a pregnancy test?
Doctors recommend testing 7 days after your missed period for the most accurate result.
2. Can I get a false negative pregnancy test?
Yes. Testing too early, diluted urine, or late implantation can all cause false negatives.
3. Should I test in the morning?
Yes. First-morning urine contains the highest hCG concentration, improving accuracy.
4. When should I see a doctor after a positive test?
Most women should schedule their first prenatal visit between 6 and 8 weeks of pregnancy.
5. Can stress cause a missed period even if I’m not pregnant?
Absolutely. Stress can disrupt hormonal balance and delay or stop ovulation.

Leave a Reply