Understanding Infertility in Men and Women
Infertility is a deeply emotional and complex issue that affects millions of couples around the world. It’s not just a medical concern; it touches the very core of relationships, self-esteem, and family dreams. Many people assume infertility is only a “female problem,” but in truth, both men and women can experience fertility issues. Understanding the different types of infertility in men and women is the first step toward addressing them effectively.
Infertility doesn’t mean a person can never have children—it simply means that achieving pregnancy may require more time, medical intervention, or lifestyle adjustments. The modern world, with its stress, environmental pollutants, and delayed parenthood trends, has contributed to rising infertility rates. But the good news is that with proper diagnosis, medical treatment, and lifestyle changes, many couples overcome these challenges successfully.
In this article, we’ll explore in detail the types of infertility in both men and women, the underlying causes, how it’s diagnosed, and available treatments. By the end, you’ll have a clearer understanding of what infertility really means—and how hope still shines through even in the toughest times.
What is Infertility? A Comprehensive Definition
Infertility is medically defined as the inability to conceive after one year of regular, unprotected sexual intercourse. For women over the age of 35, this period is often reduced to six months because fertility declines more rapidly after that age.
Infertility can be primary—when a couple has never achieved pregnancy—or secondary, where a couple has had a child before but is now unable to conceive again. The difference between these two forms lies not in the emotional pain they bring but in their medical background. Understanding the difference helps doctors recommend suitable treatment options.
Biologically, successful conception requires several steps to align perfectly:
- The woman must ovulate (release an egg).
- The man must produce healthy sperm.
- The sperm must reach and fertilize the egg.
- The fertilized egg must travel to the uterus and implant successfully.
A disruption in any of these steps can lead to infertility. Whether the cause lies with the man, the woman, or both, infertility is a shared challenge that requires empathy and teamwork to overcome.
How Common is Infertility Worldwide?
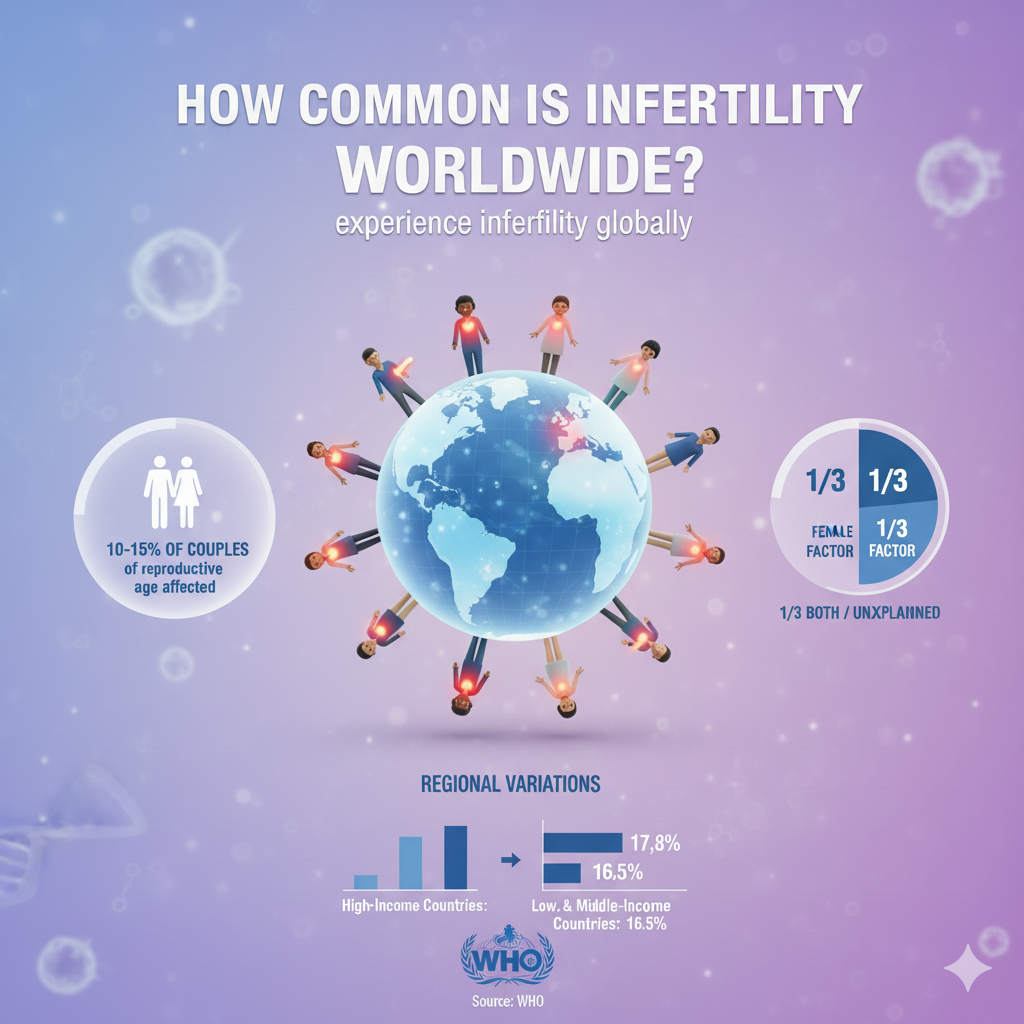
Infertility affects approximately 1 in 6 couples globally, according to the World Health Organization. That’s a significant portion of the population dealing with the inability to conceive naturally. Interestingly, studies show that male infertility contributes to about 40–50% of all infertility cases. This means infertility is not just a women’s issue—it’s equally shared.
The reasons behind rising infertility rates include:
- Delayed childbearing due to career and lifestyle choices
- Increased stress levels and poor work-life balance
- Exposure to toxins from pollution and processed foods
- Unhealthy habits, such as smoking and alcohol use
- Medical conditions like PCOS, diabetes, and obesity
Geographical factors also play a role. For instance, industrialized regions with higher pollution levels report more fertility issues. However, awareness is growing, and advances in reproductive medicine are giving hope to millions of couples every year.
Causes of Infertility in Men and Women
Infertility is a complex condition with many potential causes, and it can arise from either partner—or both. Let’s break down the primary causes based on gender.
Male Infertility Causes
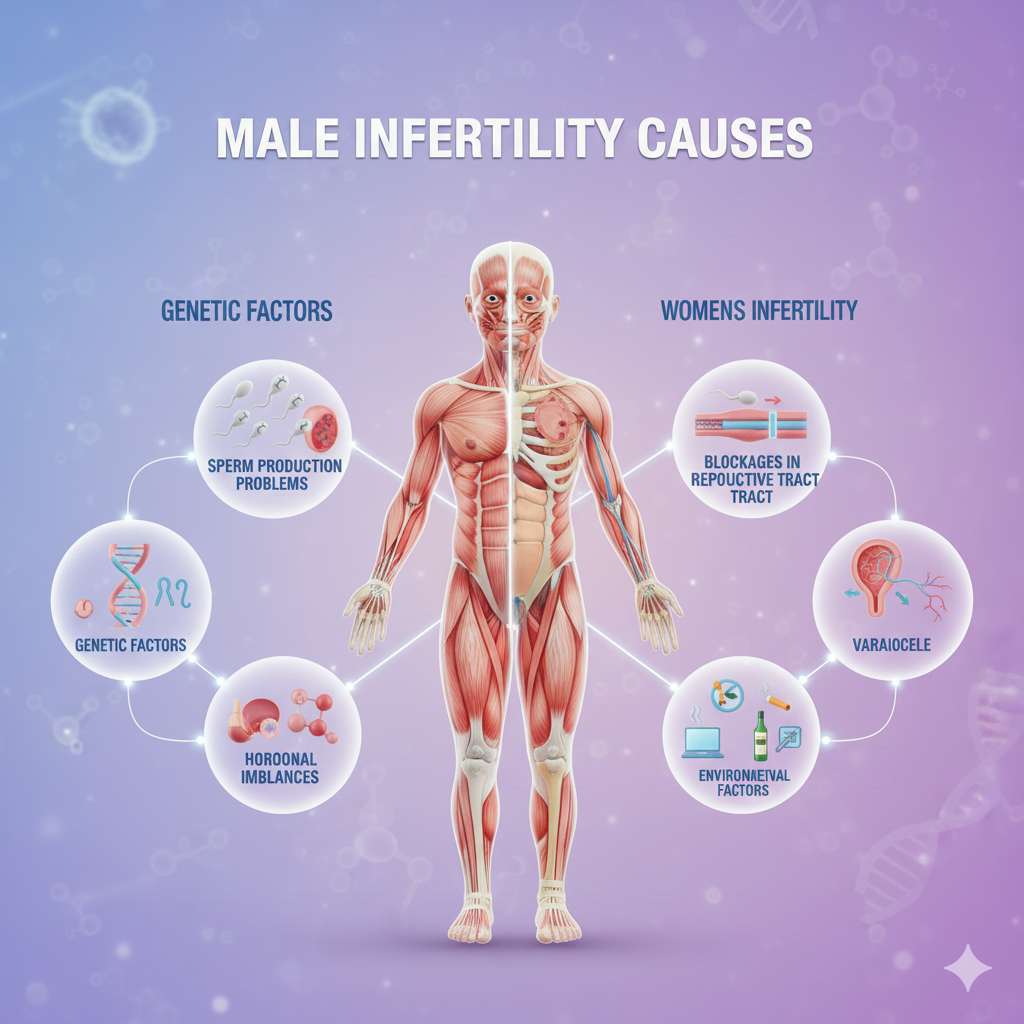
Male infertility typically stems from problems with sperm production, quality, or delivery. Common causes include:
- Low sperm count
- Poor sperm motility (movement)
- Abnormal sperm shape
- Blockages in reproductive organs
- Hormonal imbalances
- Genetic disorders
In some cases, lifestyle factors like excessive heat exposure (saunas, tight clothing), drug use, and stress can also lead to male infertility.
Female Infertility Causes
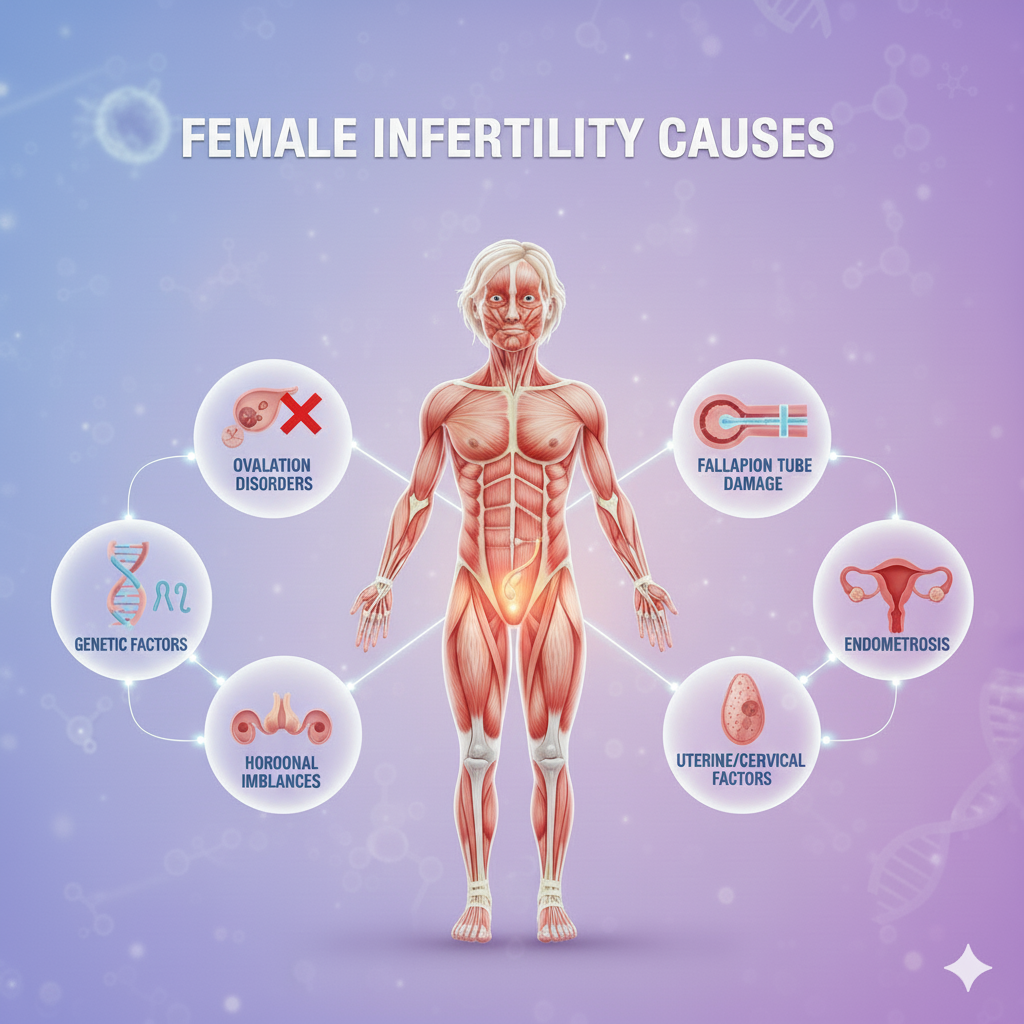
For women, infertility often relates to ovulation disorders or issues with the uterus or fallopian tubes. Common causes include:
- Ovulation problems (like PCOS)
- Endometriosis
- Tubal blockages
- Uterine abnormalities
- Hormonal imbalances
Age is another major factor—female fertility starts declining after 30 and drops significantly after 35 due to reduced egg quality and quantity.
Different Types of Infertility in Men
When discussing male infertility, doctors usually classify it into two main categories: primary and secondary infertility.
Primary Male Infertility
Primary infertility in men occurs when a man has never been able to achieve a pregnancy with any partner. This type is often caused by:
- Congenital abnormalities (like undescended testicles)
- Genetic conditions (e.g., Klinefelter’s syndrome)
- Hormonal imbalances affecting sperm production
- Testicular damage from infections, trauma, or radiation
These conditions may prevent the testicles from producing healthy, motile sperm. Early diagnosis can sometimes help manage or treat underlying causes.
Secondary Male Infertility
Secondary infertility happens when a man has fathered a child before but is now unable to do so again. This can be caused by new health problems or lifestyle changes, such as:
- Aging and declining testosterone levels
- Infections or surgeries affecting the reproductive system
- Weight gain and poor diet
- Substance abuse
- Exposure to environmental toxins
The emotional toll of secondary infertility can be just as intense as primary infertility, often leaving men confused and frustrated when fertility suddenly changes.
Common Medical Conditions Behind Male Infertility
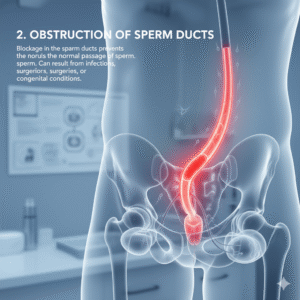
Male infertility can be linked to several medical conditions that directly affect sperm production or function. Let’s explore the most common ones and understand how each impacts male fertility.
Low Sperm Count (Oligospermia)
A low sperm count means that a man’s semen contains fewer sperm than normal. For conception, sperm count plays a vital role because fewer sperm lower the chances of fertilizing an egg. Normally, a healthy sperm count is over 15 million sperm per milliliter of semen Analysis. Anything less than that can reduce fertility.
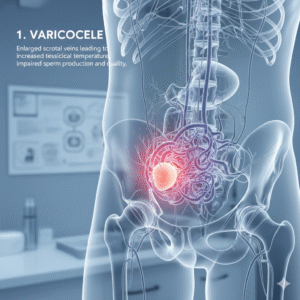
Common causes of oligospermia include hormonal imbalances, varicocele (enlarged veins in the testicles), infections, and lifestyle habits such as smoking or alcohol use. Stress and obesity can also contribute. Fortunately, treatments such as medication, surgery, or lifestyle changes can often improve sperm count.
Azoospermia (Absence of Sperm)
Azoospermia refers to a condition where no sperm are present in the ejaculate. This condition can be obstructive (due to blockages in the reproductive tract) or non-obstructive (caused by testicular failure or hormonal issues). Men with azoospermia usually have normal sexual function, which makes the diagnosis surprising and difficult emotionally.
In some cases, surgical procedures can help retrieve sperm directly from the testicles for assisted reproduction. Identifying whether it’s obstructive or non-obstructive is key to selecting the right treatment approach.
Poor Sperm Motility (Asthenozoospermia)
Even if sperm count is normal, poor motility—when sperm don’t swim effectively—can prevent them from reaching the egg. Causes include infections, varicocele, or even prolonged sitting that raises testicular temperature. Healthy sperm must be active and move forward in a straight line to reach and fertilize the egg.
Doctors usually recommend lifestyle improvements, antioxidant supplements, and sometimes assisted reproductive techniques like IVF with ICSI (Intracytoplasmic Sperm Injection) to help overcome this issue.
Abnormal Sperm Morphology (Teratozoospermia)
Morphology refers to the shape and structure of sperm. Abnormally shaped sperm—those with misshapen heads or defective tails—may have trouble penetrating the egg’s outer layer. This condition can be caused by genetic factors, smoking, toxins, or infections.
While some men with abnormal morphology can still father children naturally, severe cases often require assisted reproductive treatments.
Ejaculatory Disorders
Problems such as retrograde ejaculation (when semen enters the bladder instead of exiting through the penis) or premature ejaculation can hinder conception. These conditions might arise from nerve damage, diabetes, surgery, or certain medications. Treatments depend on the cause and may include medications or surgical corrections.
Hormonal and Genetic Factors Affecting Male Fertility
The male reproductive system relies heavily on hormones, and even a slight imbalance can disrupt sperm production. Similarly, genetic factors may influence fertility more than most realize.
Hormonal Imbalance
Testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) play crucial roles in sperm production. Any imbalance in these hormones can reduce sperm count and motility. For example, low testosterone levels can lead to decreased sperm production and libido.
Conditions such as hypogonadism or pituitary gland disorders may cause these imbalances. Hormone replacement therapy or medications that stimulate natural testosterone production can often restore balance.
Genetic Disorders and Chromosomal Abnormalities
Some men are born with genetic conditions that affect fertility. Klinefelter’s syndrome, for example, involves an extra X chromosome and leads to smaller testicles and low sperm production. Other chromosomal defects or Y-chromosome microdeletions can also impact sperm formation.
Genetic testing can identify these abnormalities. While natural conception might be difficult, assisted reproductive technologies often provide alternative paths to fatherhood.
Lifestyle and Environmental Causes of Male Infertility
Modern lifestyles have a massive impact on male fertility. Everything from what you eat to where you work can influence sperm health.
Smoking and Alcohol Consumption
Cigarettes contain toxins that damage sperm DNA and reduce motility. Similarly, alcohol lowers testosterone levels and impairs sperm production. Studies show that men who smoke or drink heavily often experience poorer sperm quality compared to those who don’t.
Reducing or eliminating these habits can significantly improve fertility. It may take a few months since sperm take around 70–90 days to regenerate fully.
Exposure to Heat and Chemicals
Frequent use of saunas, hot tubs, or even sitting with laptops on laps can increase scrotal temperature, which negatively affects sperm. Industrial workers exposed to chemicals, pesticides, or heavy metals also face higher infertility risks. Protective gear and minimizing exposure can help reduce these effects.
Obesity and Poor Diet
Being overweight affects hormone balance, leading to reduced sperm count and quality. Poor diets high in processed foods and low in vitamins and antioxidants also damage sperm DNA. Maintaining a healthy weight, eating a nutrient-rich diet, and regular exercise can drastically boost fertility.
Different Types of Infertility in Women
Female infertility can be divided into primary and secondary infertility, similar to male infertility.
Primary Female Infertility
Primary infertility occurs when a woman has never conceived despite regular unprotected intercourse. Common causes include hormonal imbalances, congenital reproductive abnormalities, and ovulation problems. Women with PCOS or endometriosis often experience primary infertility.
Secondary Female Infertility
Secondary infertility affects women who have previously conceived but now face difficulties getting pregnant again. This may be due to age-related decline in egg quality, uterine scarring from childbirth or surgery, or hormonal issues that develop later in life.
Both primary and secondary infertility can have deep emotional effects, often leaving women feeling confused and isolated. However, with modern treatments, many overcome these obstacles successfully.
Common Medical Conditions Behind Female Infertility
Ovulatory Disorders (Anovulation)
One of the most common causes of female infertility is irregular or absent ovulation. Without the release of an egg, conception is impossible. Hormonal disorders, excessive exercise, thyroid problems, and extreme stress can all disrupt ovulation.
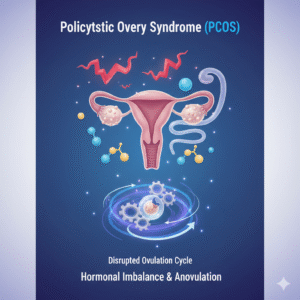
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal imbalance where the ovaries produce excessive androgens (male hormones), causing irregular cycles and multiple small cysts on the ovaries. Women with PCOS often struggle with weight gain, acne, and hair growth, along with infertility. Lifestyle management and medications like Clomiphene Citrate can help regulate ovulation.
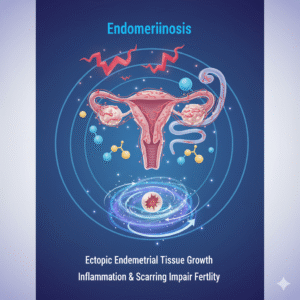
Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often causing pain and inflammation. It can lead to scarring, blockages in fallopian tubes, and difficulty with implantation. Laparoscopic surgery and hormone therapy can help manage the condition.
Blocked Fallopian Tubes
One of the most frequent structural causes of female infertility is blocked or damaged fallopian tubes. These tubes are essential for transporting the egg from the ovary to the uterus. When they are blocked—often due to pelvic inflammatory disease (PID), endometriosis, or previous infections—fertilization becomes impossible because the sperm can’t reach the egg.
Sometimes, partial blockages allow fertilization but prevent the fertilized egg from moving to the uterus, leading to ectopic pregnancy (a pregnancy outside the womb). Treatments for blocked fallopian tubes may include surgery to remove scar tissue or assisted reproductive techniques like in vitro fertilization (IVF), which bypass the tubes entirely.
Uterine Abnormalities
The uterus plays a key role in implantation and supporting pregnancy. Any structural abnormality—such as fibroids, polyps, septate uterus, or adhesions (Asherman’s syndrome)—can interfere with implantation or cause miscarriages.
Fibroids, for instance, are non-cancerous growths that can distort the uterine cavity, making it difficult for an embryo to implant. Surgical options such as myomectomy (removal of fibroids) often restore fertility. For minor abnormalities, minimally invasive procedures like hysteroscopy can help correct the issue.
Hormonal Imbalance and Female Fertility
Hormones are the silent orchestrators of the female reproductive system. Even the slightest imbalance can disturb ovulation, egg quality, or uterine lining thickness, all crucial for conception.
Thyroid Disorders
Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can interfere with menstrual cycles and ovulation. A poorly functioning thyroid can also lead to irregular or absent periods. Women with thyroid issues may experience fatigue, weight fluctuations, or mood changes, all of which can affect fertility indirectly.
Fortunately, thyroid-related infertility can often be corrected through proper medication and hormone regulation under a doctor’s guidance.
Prolactin Imbalance
Prolactin is the hormone responsible for milk production after childbirth. When its levels rise abnormally (a condition known as hyperprolactinemia), it can suppress ovulation by inhibiting the hormones FSH and LH. High prolactin levels might result from pituitary gland disorders or certain medications. Treating the root cause and using medications that normalize prolactin levels can restore fertility.
Premature Ovarian Failure (POF)
Premature ovarian failure, also known as primary ovarian insufficiency, occurs when a woman’s ovaries stop functioning normally before age 40. It’s different from early menopause because some ovarian activity may still remain. Causes can include autoimmune disorders, genetic factors, or chemotherapy.
Women with POF have low estrogen levels and irregular or absent periods. Although natural conception becomes challenging, donor egg IVF often provides a successful alternative.
Lifestyle and Environmental Causes of Female Infertility
Infertility isn’t always rooted in medical issues. In many cases, daily habits, diet, and emotional health play major roles.
Stress and Mental Health
Chronic stress can disrupt the delicate hormonal balance required for ovulation. High levels of cortisol (the stress hormone) can affect reproductive hormones like estrogen and progesterone. In severe cases, stress can lead to anovulation—a condition where the ovaries stop releasing eggs.
Mindfulness, yoga, and therapy can help reduce stress levels and support reproductive health. Managing emotional wellbeing is often just as vital as medical treatments in fertility journeys.
Obesity and Underweight Issues
Body weight affects fertility because it influences estrogen levels. Women who are significantly overweight or underweight often have irregular menstrual cycles or no ovulation at all. Excess fat tissue increases estrogen levels, confusing the hormonal signals that regulate ovulation.
Losing or gaining even 5–10% of body weight can often restore regular cycles and improve fertility outcomes. Maintaining a balanced diet rich in fruits, vegetables, and healthy fats supports reproductive health.
Smoking, Alcohol, and Drug Use
Smoking damages the ovaries and accelerates egg loss, leading to earlier menopause. Alcohol and recreational drugs, meanwhile, affect hormone regulation and egg quality. Quitting these habits not only boosts fertility but also improves overall health and future pregnancy outcomes.
Unexplained Infertility: When the Cause Remains Unknown
Sometimes, after all tests and evaluations, doctors find no clear medical explanation for infertility. This is known as unexplained infertility, and it affects about 10–20% of couples struggling to conceive.
Unexplained infertility doesn’t mean there’s no problem—it just means current medical technology hasn’t pinpointed it yet. Factors like minor sperm abnormalities, subtle hormonal shifts, or issues with egg quality could be involved.
Treatment usually focuses on increasing the chances of conception using methods like ovulation stimulation, intrauterine insemination (IUI), or IVF. Even without a clear diagnosis, many couples eventually succeed with persistence and support.
Diagnosis of Infertility in Men and Women
Accurate diagnosis is the cornerstone of successful fertility treatment. Since infertility can stem from either partner—or both—both must undergo evaluation.
Tests for Men
- Semen Analysis: The first and most common test that evaluates sperm count, motility, and morphology.
- Hormone Testing: Checks testosterone and FSH levels to assess hormonal health.
- Genetic Testing: Detects chromosomal abnormalities affecting sperm production.
- Scrotal Ultrasound: Identifies structural issues such as varicocele or blockages.
- Testicular Biopsy: In some cases, tissue samples are analyzed to confirm sperm production.
Tests for Women
- Ovulation Testing: Blood tests for progesterone confirm whether ovulation occurs.
- Ultrasound Scan: Assesses ovarian function, egg development, and uterine health.
- Hysterosalpingography (HSG): HSG test procedure that examines fallopian tube patency.
- Laparoscopy: A minor surgical procedure to detect endometriosis or pelvic scarring.
- Hormonal Profile: Evaluates levels of FSH, LH, estrogen, and thyroid hormones.
Each test helps narrow down the root cause, guiding doctors to choose effective treatment strategies.
Treatment Options for Different Types of Infertility
Medications
For many couples, fertility medications are the first line of treatment. Drugs like Clomiphene Citrate, Letrozole, or Gonadotropins stimulate ovulation in women, while hormone therapy may help men with low testosterone or hormonal imbalances.
Surgical Treatments
Surgery can correct structural problems like blocked fallopian tubes, fibroids, or varicocele in men. Laparoscopic and hysteroscopic procedures are minimally invasive options that restore normal anatomy and improve fertility chances.
Assisted Reproductive Technologies (ART)
ART includes advanced fertility treatments such as:
- Intrauterine Insemination (IUI): Sperm is placed directly into the uterus to improve chances of fertilization.
- In Vitro Fertilization (IVF): Eggs are fertilized in a lab and then implanted into the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected into an egg during IVF—often used for male infertility.
- Egg or Sperm Donation: For couples facing severe fertility issues, donor gametes offer a path to parenthood.
Prevention and Lifestyle Modifications to Improve Fertility
Preventing infertility often starts with everyday choices. Maintaining a balanced diet, regular exercise, and a stress-free lifestyle are crucial. Avoiding smoking, limiting alcohol, and keeping a healthy body weight can make a big difference.
For men, wearing loose clothing and avoiding prolonged heat exposure protects sperm quality. For women, tracking ovulation, managing weight, and regular gynecological checkups help preserve fertility.
Emotional and Psychological Impact of Infertility
Infertility can take a serious emotional toll. Feelings of guilt, frustration, and anxiety are common, especially when conception takes longer than expected. Couples often face social pressure or isolation.
Emotional support, counseling, and joining infertility support groups can help manage stress. Remember, fertility challenges are a shared journey—communication, patience, and compassion strengthen relationships during these tough times.
When to See a Fertility Specialist
It’s advisable to seek professional help if:
- You’ve been trying to conceive for over a year (or 6 months if over 35).
- You have irregular periods or a history of reproductive disorders.
- You’ve experienced multiple miscarriages.
- You have known risk factors such as PCOS, endometriosis, or testicular issues.
Early intervention increases the chances of successful treatment and conception.
Hope and Possibilities for Couples Facing Infertility
Infertility, while challenging, is not the end of the road. Advances in reproductive medicine mean that even the most complex cases can often be treated successfully. Whether it’s through medication, lifestyle adjustments, or advanced reproductive technologies, countless couples worldwide are achieving their dreams of parenthood.
The key is awareness, patience, and timely medical guidance. Infertility may test a couple’s resilience, but it can also strengthen their bond and determination to create life together.
FAQs
- Can infertility be cured naturally?
In some cases, lifestyle changes like weight management, stress reduction, and a balanced diet can significantly improve fertility without medical intervention. - Does age affect male fertility too?
Yes, sperm quality declines gradually with age, affecting motility and DNA integrity, though men remain fertile longer than women. - How long should couples try before seeing a doctor?
If under 35, try for a year. If over 35, seek medical advice after 6 months of trying. - Can stress really cause infertility?
Chronic stress can disrupt hormonal balance and ovulation cycles, indirectly contributing to infertility. - Are IVF and ICSI safe treatments?
Yes. They are widely used and have high success rates, though outcomes depend on age, health, and specific fertility conditions.


Leave a Reply