Introduction to Skin Rash
Definition of Skin Rash
A skin rash is a noticeable change in the color, texture, or appearance of the skin, often accompanied by itching, irritation, or discomfort. It may appear as redness, bumps, blisters, or patches and can affect any part of the body. While most rashes are temporary and harmless, others may indicate underlying medical conditions. Skin rashes can result from allergies, infections, medications, or even lifestyle factors. Understanding rashes is essential because early identification and management can prevent discomfort, complications, and spread of infections.
Why Understanding Skin Rash is Important
Skin is the body’s largest organ, and it acts as the first line of defense against harmful pathogens and irritants. A rash is often the skin’s way of signaling that something is wrong—whether it’s an allergy, an infection, or an autoimmune reaction. Ignoring persistent rashes can lead to worsening conditions, spreading infections, or even systemic health issues. For example, a simple allergic rash can progress into severe eczema, or untreated bacterial rashes can lead to cellulitis. Recognizing the type, cause, and symptoms of a rash helps in timely treatment and prevention.
Common Types of Skin Rash
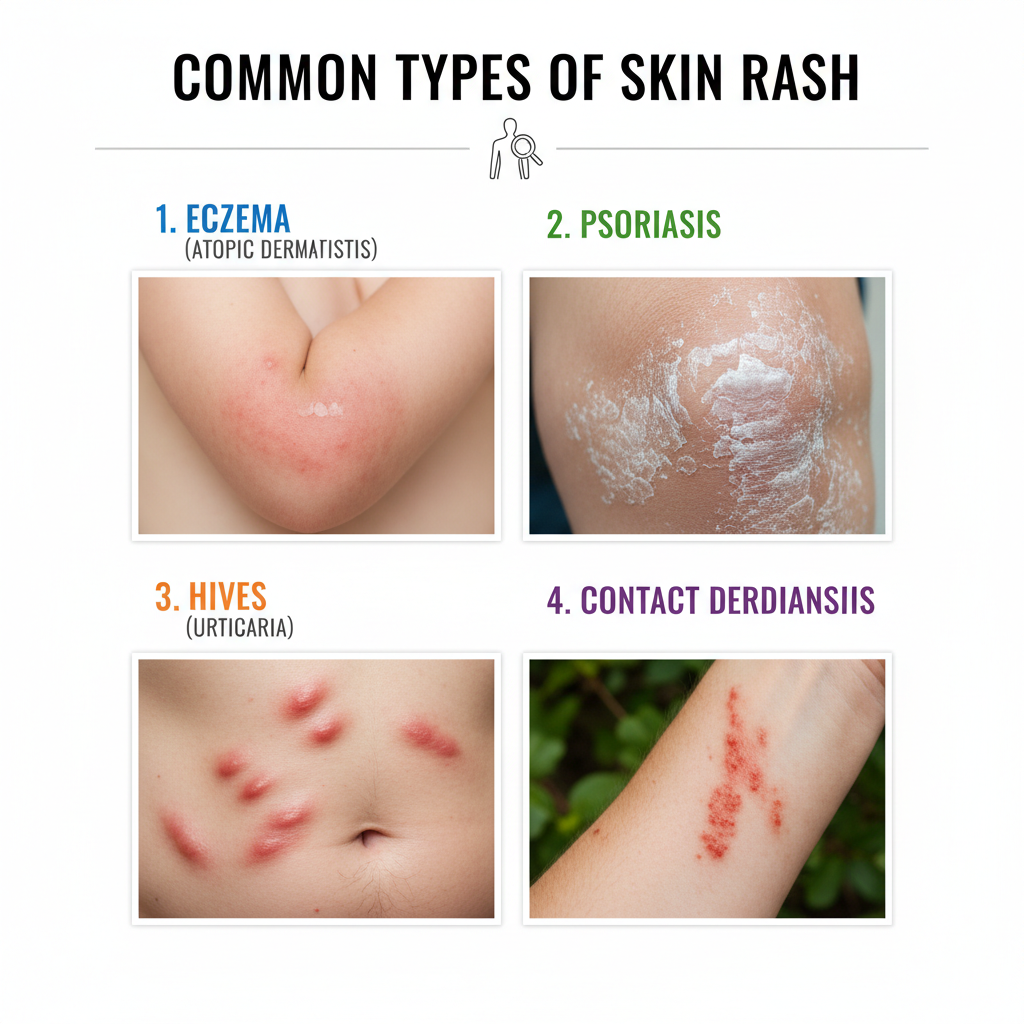
Eczema (Atopic Dermatitis)
Eczema is a chronic condition characterized by dry, itchy, inflamed patches of skin. It often appears on the face, elbows, knees, or hands and may flare up periodically. Triggers include allergens, soaps, stress, and environmental factors. The condition is linked to an overactive immune response and often runs in families. Eczema causes persistent discomfort and may lead to skin infections due to scratching. Treatments include moisturizers, corticosteroid creams, antihistamines, and lifestyle changes such as avoiding harsh detergents and maintaining skin hydration.
Psoriasis
Psoriasis is an autoimmune skin disorder that speeds up the life cycle of skin cells, causing thick, scaly patches. These patches are often red, covered with silvery scales, and may appear on the scalp, elbows, knees, or lower back. Unlike eczema, psoriasis is not triggered by allergens but by immune system dysfunction. Flare-ups can be influenced by stress, cold weather, and infections. Treatment includes topical ointments, phototherapy, and systemic medications. Managing psoriasis requires long-term care, as it is a recurring condition.
Contact Dermatitis
Contact dermatitis occurs when the skin reacts to direct contact with an irritant or allergen. Common irritants include soaps, detergents, perfumes, and metals like nickel. Allergic contact dermatitis happens when the immune system reacts to allergens such as poison ivy or certain cosmetics. Symptoms include redness, itching, swelling, and sometimes blistering. The best treatment is avoiding the triggering substance and using soothing creams or antihistamines to reduce symptoms.
Heat Rash (Prickly Heat)
Heat rash, or prickly heat, appears when sweat glands get blocked, trapping sweat under the skin. This causes red, itchy bumps, often accompanied by a prickling sensation. It usually develops in hot, humid conditions and affects areas like the neck, chest, and back. Babies and people who sweat excessively are more prone to it. Wearing loose cotton clothes, keeping the skin cool, and using soothing powders can help manage heat rash.
Hives (Urticaria)
Hives are raised, itchy welts that appear suddenly on the skin, often due to allergic reactions. They may be triggered by foods, insect bites, medications, or stress. Hives can last a few hours to several days and may change shape or move across the body. Severe cases can involve swelling of the lips, tongue, or throat, requiring immediate medical attention. Antihistamines are commonly used for relief, and identifying triggers helps prevent recurrence.
Causes of Skin Rash

Allergic Reactions
Allergic reactions are among the most common causes of skin rashes. They occur when the immune system mistakenly identifies harmless substances—such as pollen, dust, certain foods, or chemicals—as threats. Contact with these allergens triggers the release of histamines, leading to redness, itching, and swelling. Common allergic rashes include hives and contact dermatitis. Managing allergies involves avoiding triggers, using antihistamines, and keeping the skin moisturized to reduce sensitivity.
Infections (Viral, Bacterial, Fungal, Parasitic)
Infections are another significant cause of skin rashes. Viral infections such as measles, chickenpox, or shingles often present with widespread rashes. Bacterial infections like impetigo cause crusty, yellowish sores, while cellulitis leads to painful swelling and redness. Fungal infections, such as ringworm and athlete’s foot, cause circular, scaly patches. Parasitic infections, like scabies, result in intense itching and burrows on the skin. Identifying the type of infection is essential for appropriate treatment, as antifungals, antivirals, and antibiotics differ in application.
Environmental Factors
Environmental conditions like heat, humidity, pollution, or extreme cold can trigger rashes. For example, heat rash develops in hot, sweaty conditions, while cold weather can dry out the skin and cause eczema flare-ups. Sun exposure can lead to sunburn and rashes known as photodermatitis. Wearing protective clothing, using sunscreen, and maintaining proper skincare routines can reduce environmental rash triggers.
Autoimmune Disorders
In autoimmune conditions, the immune system attacks healthy skin cells, leading to chronic rashes. Psoriasis and lupus are prime examples. In lupus, a distinctive butterfly-shaped rash may appear on the face. Autoimmune rashes require medical management with immunosuppressants, corticosteroids, or biologic drugs. Early diagnosis helps prevent complications and organ involvement in systemic autoimmune diseases.
Genetic Factors
Some people are genetically predisposed to skin rashes. For example, eczema often runs in families with a history of asthma or hay fever. Genetic mutations affecting skin barriers make individuals more susceptible to irritation and infection. While genetic causes cannot be eliminated, preventive care, regular moisturization, and avoiding triggers help manage the condition effectively.
Symptoms of Skin Rash
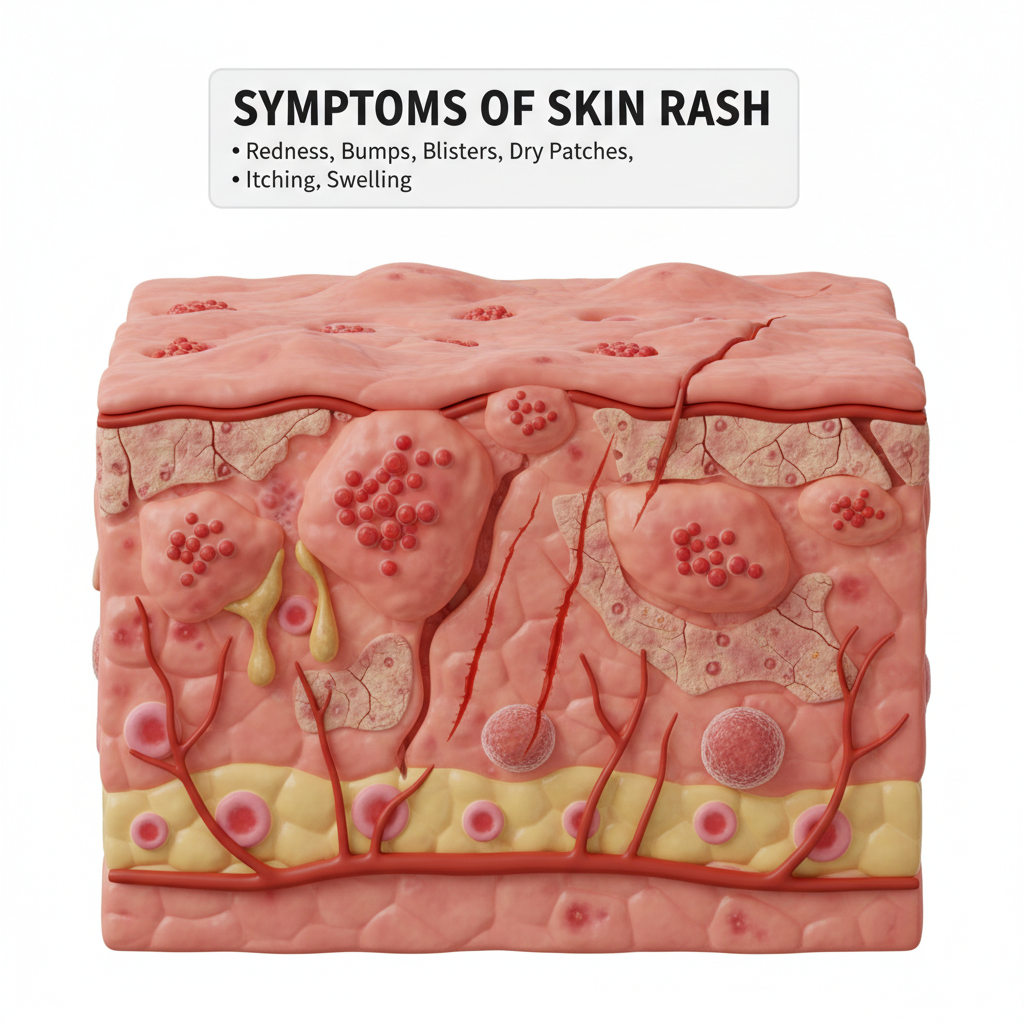
Redness and Inflammation
Redness is the most common symptom of skin rash, signaling irritation, infection, or inflammation. The skin may appear blotchy or uniformly red, depending on the type of rash. Inflammation often accompanies redness, making the skin warm to the touch. Redness is a visible marker but not specific to any one condition, so identifying accompanying symptoms helps determine the underlying cause.
Itching and Burning Sensation
Itching is perhaps the most distressing symptom of a skin rash. It can range from mild irritation to intense, uncontrollable scratching that worsens the rash. Some conditions, like eczema and hives, cause intense itching, while fungal infections may produce both itching and burning sensations. Scratching not only worsens the irritation but also increases the risk of infection, making it important to manage itching with medications or soothing remedies.
Dryness, Crusting, and Scaling
Certain rashes lead to excessive dryness and flaking of the skin. Conditions like psoriasis and eczema cause scaling, where thickened layers of skin peel off. In bacterial infections, crusting may occur as pus dries over sores. Dry, scaly rashes are often chronic and require ongoing moisturization, medicated creams, and gentle skincare routines.
Blisters, Pustules, and Oozing
Some rashes progress to blisters filled with fluid or pus. Viral rashes like chickenpox and shingles are known for blister formation, while bacterial infections may lead to pus-filled lesions. Oozing from rashes indicates infection or severe irritation. Keeping the affected area clean and covered helps prevent secondary infections and promotes healing.
Pain and Discomfort
Not all rashes itch; some cause pain or tenderness. Shingles, for instance, produces painful blisters along nerve lines. Cellulitis causes deep pain due to skin and tissue inflammation. Persistent pain with rashes may indicate a serious condition requiring medical intervention.
Diagnosis and Tests for Skin Rash
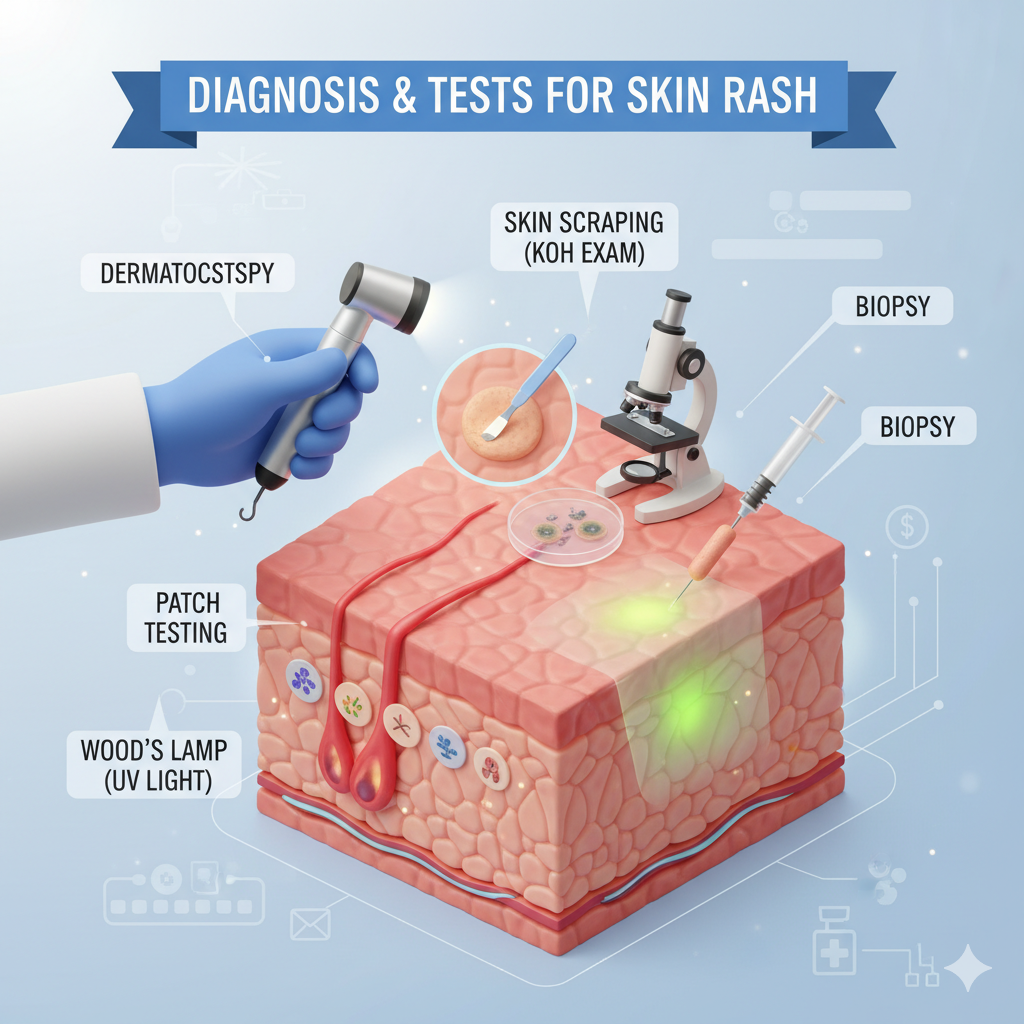
Physical Examination
Doctors usually start with a thorough physical exam of the rash, noting its location, color, texture, and spread. Some rashes have distinctive appearances, such as ring-shaped patches in fungal infections or the butterfly rash of lupus.
Medical History Evaluation
A detailed history helps identify possible triggers such as new medications, recent infections, or contact with irritants. Family history may also reveal genetic predispositions.
Patch Testing for Allergies
Patch testing involves placing small amounts of allergens on the skin to check for reactions. This test helps identify substances causing allergic contact dermatitis.
Skin Biopsy
In complex cases, a small sample of the rash is taken for microscopic examination. This helps confirm conditions like psoriasis, lupus, or skin cancer.
Blood Tests for Underlying Conditions
Blood tests may be ordered if autoimmune diseases, infections, or systemic issues are suspected. For instance, elevated markers of inflammation may point to lupus or rheumatoid arthritis.
Treatment Options for Skin Rash
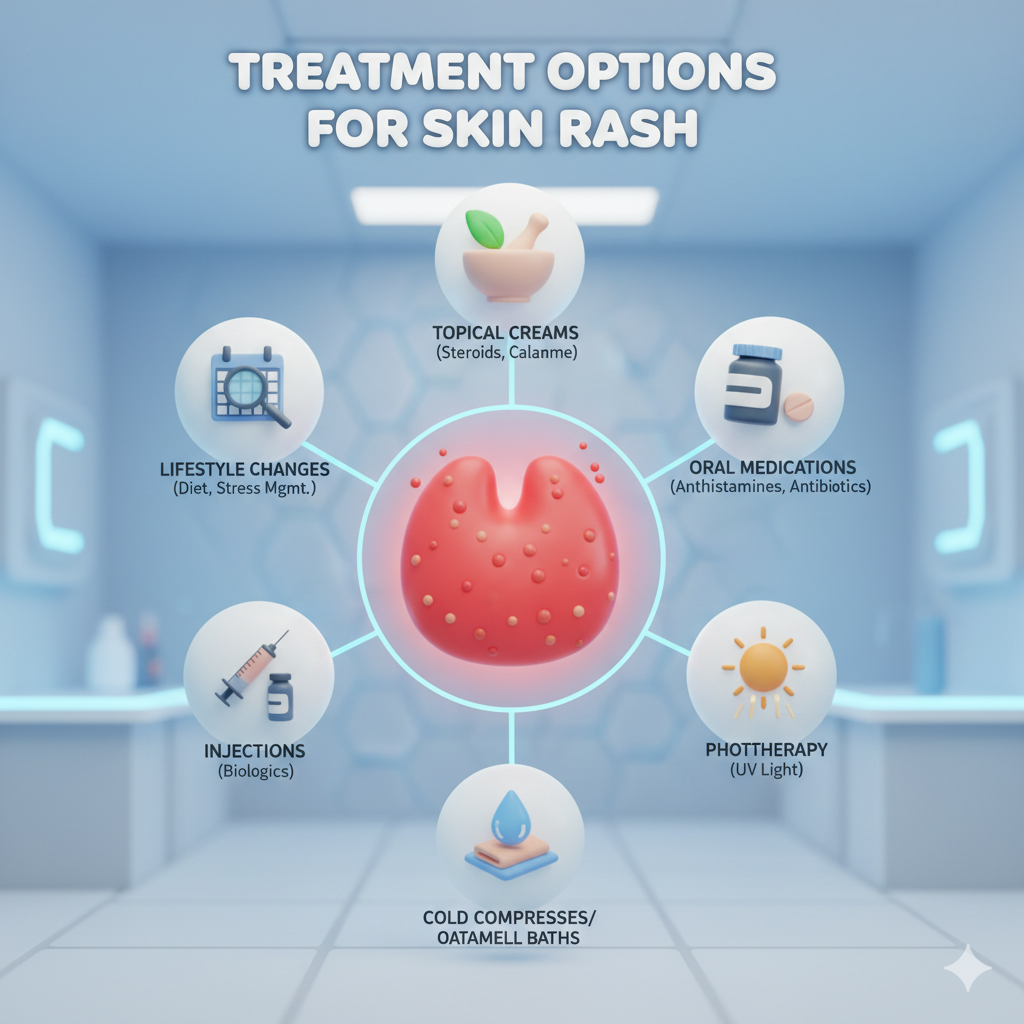
Home Remedies and Self-Care
For many mild rashes, home remedies provide significant relief. Keeping the affected area clean and dry is the first step. Gentle cleansing with lukewarm water helps remove irritants without stripping the skin’s natural oils. Applying cold compresses reduces itching and swelling, while avoiding hot showers prevents further irritation. Loose cotton clothing prevents friction and allows the skin to breathe. Moisturizers, especially fragrance-free ones, lock in hydration and reduce dryness. Natural remedies like aloe vera gel and oatmeal baths soothe inflammation. It’s also important to avoid scratching, as this worsens the rash and increases infection risks. If the rash is allergy-related, identifying and avoiding the trigger—whether it’s a detergent, food, or fabric—is crucial.
Over-the-Counter Medications
When home remedies aren’t enough, over-the-counter (OTC) medications can help manage symptoms. Hydrocortisone creams reduce redness and itching in mild rashes, while antihistamines like loratadine or diphenhydramine relieve allergic reactions. Antifungal creams are effective for ringworm and athlete’s foot, while antibacterial ointments help prevent infection in minor cuts and rashes. Calamine lotion is widely used to soothe insect bites and chickenpox-related itching. These medications are easily available, but it’s essential to follow instructions carefully and avoid overuse, which can thin the skin or cause resistance in infections.
Prescription Medications (Topical & Oral)
For severe or persistent rashes, doctors may prescribe stronger medications. Topical corticosteroids are used for eczema and psoriasis, while oral antihistamines treat stubborn allergic reactions. Antibiotics may be prescribed for bacterial infections like cellulitis, and antifungal pills for widespread fungal infections. Immunosuppressants or biologics are sometimes necessary for autoimmune-related rashes like psoriasis or lupus. These treatments target the underlying cause and provide long-term relief but must be monitored for side effects. Patients should take doctor consultation and complete the prescribed course of treatment to avoid recurrence.
Lifestyle Changes and Prevention
Long-term skin health depends on lifestyle choices. A balanced diet rich in vitamins and omega-3 fatty acids strengthens the skin barrier. Drinking plenty of water keeps the skin hydrated. Reducing stress through yoga, meditation, or exercise helps prevent stress-induced rashes. Avoiding harsh soaps, strong detergents, and excessive sun exposure reduces skin irritation. Regular moisturizing, gentle skincare products, and proper hygiene go a long way in preventing flare-ups. Prevention is always better than cure, especially for chronic skin conditions.
Natural Remedies for Skin Rash Relief

Aloe Vera
Aloe vera is known for its cooling and healing properties. Fresh aloe vera gel reduces redness, itching, and inflammation. It also provides moisture, which is essential for conditions like eczema and psoriasis. Aloe contains compounds that promote wound healing and prevent bacterial growth, making it a safe natural remedy for various rashes. Applying it directly from the plant ensures purity and effectiveness.
Coconut Oil
Coconut oil acts as both a moisturizer and an antimicrobial agent. Its fatty acids help soothe dry, irritated skin while reducing inflammation. It is particularly useful for eczema and fungal infections. Unlike petroleum-based moisturizers, coconut oil penetrates the skin deeply, providing lasting hydration. Applying it at night allows better absorption and helps restore the skin’s protective barrier.
Oatmeal Baths
Oatmeal has natural anti-inflammatory and antioxidant properties that calm irritated skin. Colloidal oatmeal, when added to lukewarm bathwater, creates a soothing effect, reducing itching and redness. This remedy is especially effective for chickenpox, hives, and eczema flare-ups. Regular oatmeal baths help maintain soft, hydrated skin and relieve discomfort from various rashes.
Herbal Teas and Compresses
Certain herbal teas, like chamomile and green tea, can be used topically as compresses to reduce inflammation. Chamomile has calming effects, while green tea contains antioxidants that promote healing. Simply soaking a clean cloth in cooled tea and applying it to the rash can bring relief. These natural remedies are gentle alternatives for those with sensitive skin who want to avoid chemical-based treatments.
When to See a Doctor for Skin Rash
Persistent Rash
If a rash lasts more than a week without improvement despite home care, it’s time to see a doctor. Persistent rashes may signal underlying conditions such as eczema, psoriasis, or autoimmune disorders. Early medical attention helps prevent complications and ensures proper treatment.
Severe Pain or Swelling
Not all rashes are just itchy or uncomfortable—some cause significant pain or swelling. A painful rash could indicate shingles, cellulitis, or other serious infections. If swelling spreads or becomes severe, immediate medical care is essential to avoid complications.
Accompanied by Fever or Breathing Issues
When a rash appears with fever, chills, or breathing difficulties, it could signal a systemic allergic reaction, measles, or other serious infections. Conditions like anaphylaxis require urgent treatment. If you experience difficulty breathing, swelling of the face or throat, or high fever, emergency care is critical.
Complications of Untreated Skin Rash
Secondary Infections
Scratching an itchy rash often leads to open wounds, which can get infected by bacteria. This results in pus-filled sores, crusting, and sometimes spreading infections like cellulitis. Untreated infections may require antibiotics and can worsen rapidly.
Skin Thickening and Scarring
Chronic scratching causes the skin to thicken, darken, or scar over time. This condition, known as lichenification, is common in untreated eczema. Scarring may become permanent if not managed early. Proper treatment and avoiding scratching help prevent long-term damage.
Chronic Itching and Discomfort
Ongoing rashes can cause constant itching, pain, and irritation. This not only affects daily activities but also impacts mental well-being. Untreated chronic conditions like psoriasis and eczema can severely reduce quality of life, making timely care essential.
Preventive Measures for Skin Rash
Proper Skincare Routine
A gentle skincare routine plays a vital role in rash prevention. Using fragrance-free cleansers and moisturizers reduces irritation. Regularly applying sunscreen protects against sun-induced rashes. Avoiding over-exfoliation prevents skin barrier damage.
Avoiding Triggers
Identifying and avoiding rash triggers is one of the most effective preventive strategies. For allergy-prone individuals, keeping track of products, foods, and environmental factors helps reduce flare-ups. Wearing breathable fabrics, avoiding strong detergents, and reducing contact with known irritants are practical steps.
Balanced Diet and Hydration
Nutrition plays a crucial role in skin health. A diet rich in antioxidants, vitamins A, C, and E, and omega-3 fatty acids supports skin regeneration. Staying hydrated maintains skin elasticity and prevents dryness, which can trigger rashes. Healthy skin starts from within, and consistent dietary habits can significantly reduce rash frequency.
Skin Rash in Children vs. Adults
Common Pediatric Rashes
Children are particularly prone to skin rashes because their immune systems are still developing, and their skin is more delicate than that of adults. Some of the most common rashes in children include diaper rash, chickenpox, hand-foot-and-mouth disease, and fifth disease. Diaper rash occurs due to prolonged exposure to moisture, irritants, and friction. Chickenpox presents with itchy, blister-like rashes that spread quickly across the body. Hand-foot-and-mouth disease causes red spots and blisters around the mouth, hands, and feet, while fifth disease leads to a bright red rash on the cheeks. Most pediatric rashes are viral and self-limiting but require careful monitoring to prevent secondary infections from scratching. Parents are often advised to use mild cleansers, keep the skin dry, and apply soothing ointments.
Rashes in Adults and Elderly
While children frequently get viral rashes, adults and the elderly often deal with chronic or systemic skin conditions. Shingles is a prime example, typically affecting older adults who previously had chickenpox. It presents as painful blisters along nerve pathways and requires antiviral medications. Adults may also develop eczema, psoriasis, or contact dermatitis due to long-term exposure to irritants or weakened immune function. The elderly, with thinning skin and reduced oil production, often experience dryness-related rashes that can lead to persistent itching and cracking. Unlike children, adults may face rashes linked to underlying chronic conditions such as diabetes or autoimmune disorders, making diagnosis more complex.
Differences in Symptoms and Treatment
The differences between rashes in children and adults primarily lie in causes and management. Pediatric rashes are often acute and viral, while adult rashes tend to be chronic or autoimmune in nature. Treatment in children focuses on comfort, hydration, and preventing scratching, whereas adults may require long-term medications, lifestyle changes, and ongoing dermatological care. Elderly patients often need extra hydration, gentle skincare, and close monitoring for complications like infections. Recognizing these differences helps in tailoring effective treatment approaches across age groups.
Skin Rash and Mental Health Connection
Stress-Induced Rashes
Stress doesn’t just affect the mind—it manifests physically too. When you’re under stress, your body releases hormones like cortisol that disrupt the immune system and increase inflammation. This can lead to stress-induced rashes, including hives, eczema flare-ups, or psoriasis outbreaks. People often notice these rashes during exams, work deadlines, or emotional turmoil. The skin reacts almost as a mirror to mental health, reminding us that body and mind are deeply connected. Managing stress through meditation, deep breathing, or even regular exercise can prevent flare-ups. Stress reduction isn’t just good for your mind—it’s also one of the best remedies for keeping skin healthy.
Psychological Impact of Chronic Rashes
Living with a chronic rash like eczema or psoriasis can be mentally draining. Constant itching, visible skin changes, and discomfort often lower self-esteem and lead to social anxiety. People may avoid public gatherings or feel embarrassed about their skin, which can spiral into depression or isolation. Studies show a strong link between dermatological conditions and mental health disorders such as anxiety and depression. Addressing skin health alone isn’t enough—patients often benefit from counseling, support groups, and stress management therapies alongside medical treatment. By treating the mind and the skin together, patients can achieve better long-term outcomes.
Myths and Facts about Skin Rashes
Common Misconceptions
There are many myths about skin rashes that create confusion. One common belief is that all rashes are contagious—this isn’t true. Conditions like eczema and psoriasis are not spread from person to person. Another myth is that scratching a rash makes it go away, but in reality, it worsens the irritation and increases the risk of infection. Some people think natural remedies alone can cure all rashes, but while helpful, many rashes require medical treatment. Another misconception is that rashes always indicate poor hygiene. In reality, autoimmune or allergic rashes have nothing to do with cleanliness.
Evidence-Based Facts
Science tells us that rashes can stem from multiple causes—genetic, allergic, infectious, or autoimmune. While some rashes are contagious, like ringworm and scabies, many others are not. Moisturizing regularly and avoiding irritants are proven preventive measures. Stress management plays a key role in preventing flare-ups, especially in eczema and psoriasis. It’s also a fact that untreated rashes can lead to complications such as secondary infections. Understanding these truths helps people approach skin health more wisely and avoid unnecessary stigma or incorrect treatments.
Conclusion
Skin rashes are a common health issue, but their causes, symptoms, and treatments vary widely. From temporary irritations like heat rash to chronic conditions like eczema and psoriasis, rashes are the skin’s way of signaling distress. Proper identification, timely treatment, and preventive care can significantly improve outcomes. While some rashes resolve on their own, others may indicate deeper health concerns that need medical attention. Lifestyle changes, natural remedies, and stress management are equally important alongside medical treatments. By understanding skin rashes more deeply, individuals can take better care of their skin, reduce complications, and improve overall well-being.
FAQs on Skin Rash
Q1: Can stress cause skin rash?
Yes, stress can trigger or worsen skin conditions such as hives, eczema, and psoriasis due to hormonal imbalances and immune system changes.
Q2: Are skin rashes contagious?
Not all rashes are contagious. Fungal infections, scabies, and viral rashes like chickenpox can spread, but eczema, psoriasis, and allergic rashes cannot.
Q3: How long do skin rashes usually last?
It depends on the cause. Allergic rashes may disappear within days once the trigger is removed, while chronic conditions like psoriasis can persist for months or even years.
Q4: What foods trigger skin rashes?
Common triggers include dairy, nuts, shellfish, gluten, and processed foods. However, triggers vary by individual and should be identified through careful observation or allergy test.
Q5: Can skin rash heal on its own?
Yes, mild rashes like heat rash or minor allergic reactions often resolve naturally. However, persistent, painful, or spreading rashes require medical evaluation.


Leave a Reply