Introduction to HSG Test
What is an HSG Test?
An HSG test, also known as hysterosalpingography, is a specialized X-ray procedure that evaluates a woman’s reproductive system, particularly the uterus and fallopian tubes. The test involves injecting a contrast dye into the uterus and fallopian tubes, followed by X-ray imaging to track the flow of the dye. This process helps doctors determine if the fallopian tubes are open and whether the uterus has a healthy shape for carrying a pregnancy. Unlike a standard ultrasound, which provides only structural details, the HSG test offers a clear visual of the pathways necessary for conception.
For couples struggling to conceive, this test is often one of the first diagnostic steps because it directly assesses the physical factors that may prevent pregnancy. It doesn’t just show if the tubes are blocked; it also gives valuable insight into uterine health, which is crucial for embryo implantation. Essentially, the HSG acts as a roadmap for fertility specialists, guiding them toward the right treatment plan.
Importance of HSG in Fertility Diagnosis
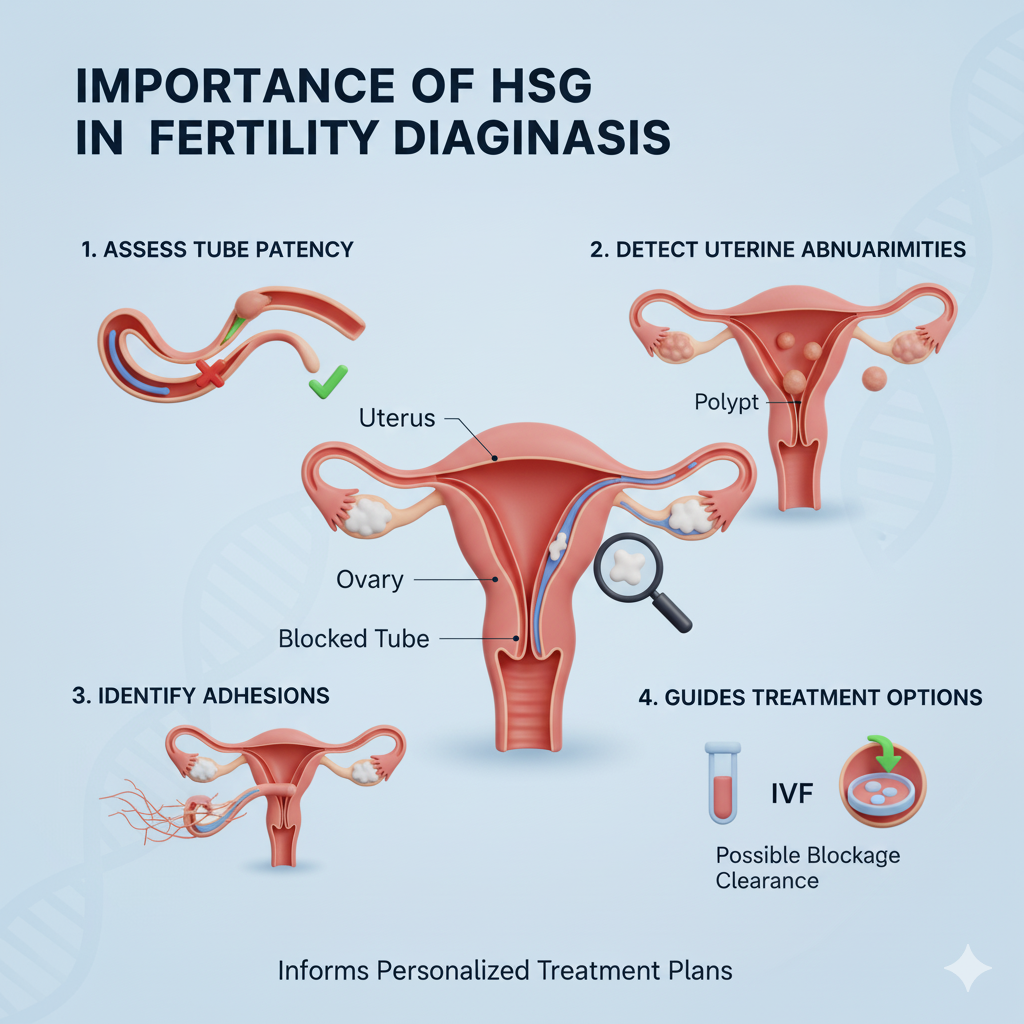
The importance of HSG test in infertility cannot be overstated. About 30-40% of infertility cases in women are linked to issues with the fallopian tubes. Since fertilization takes place inside the fallopian tube, any blockage or scarring can prevent the sperm from meeting the egg. The HSG test identifies these issues early, helping doctors decide whether natural conception is possible or if assisted reproductive techniques such as IVF (In Vitro Fertilization) or IUI (Intrauterine Insemination) are required.
Apart from tubal health, the HSG test also evaluates the uterine cavity. A uterus with an irregular shape, fibroids, polyps, or scar tissue may prevent implantation or increase the risk of miscarriage. By identifying these abnormalities, doctors can take corrective measures before suggesting fertility treatments. This is why the test is often recommended before starting costly procedures—so that hidden barriers are not overlooked.
How HSG Differs from Other Infertility Tests
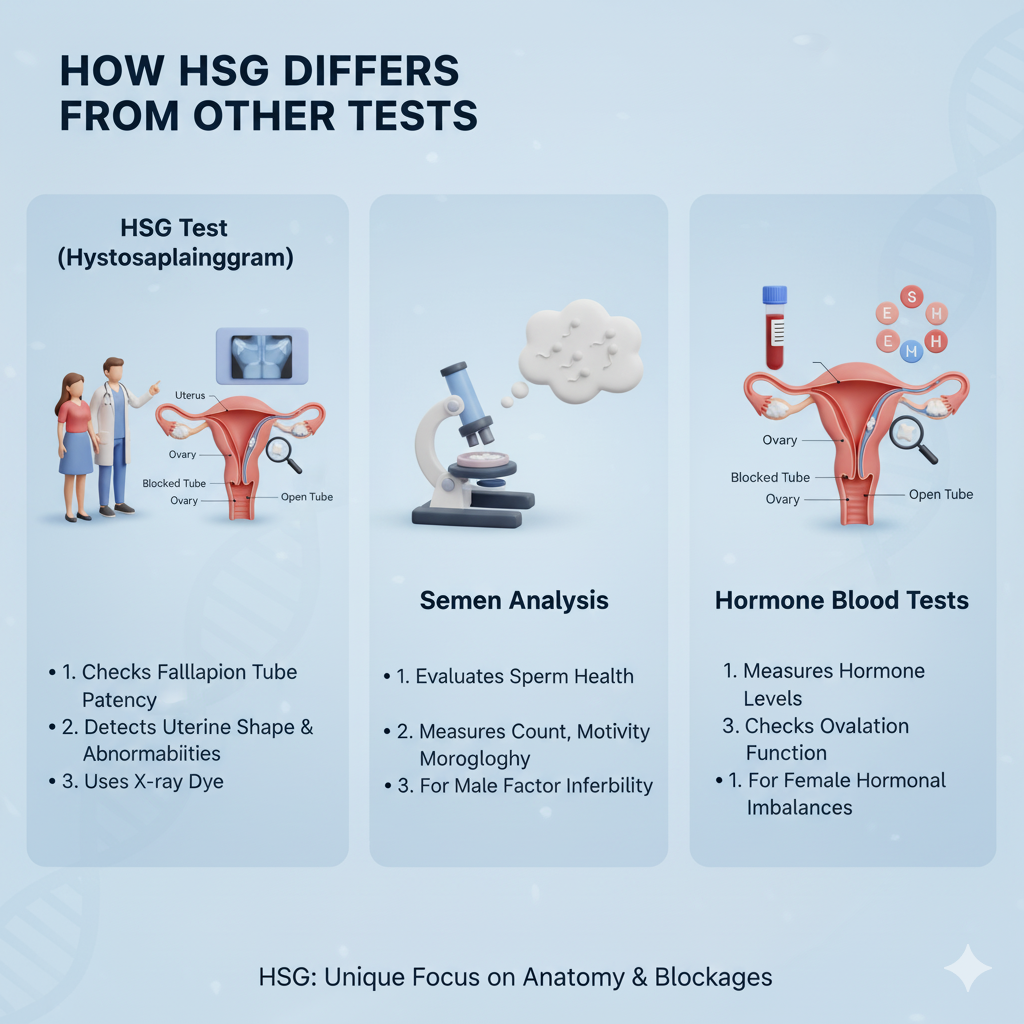
While blood tests and hormonal assessments reveal how well the ovaries are functioning, they don’t provide insights into the structural health of the reproductive system. Similarly, ultrasounds and pelvic scans are useful, but they may not clearly show blockages in the fallopian tubes. That’s where the HSG test stands out—it specifically looks at the physical condition of the pathways required for conception.
Compared to laparoscopy, another method for checking tubal health, HSG is less invasive, quicker, and often less expensive. It’s performed on an outpatient basis and usually takes less than 30 minutes. While laparoscopy requires anesthesia and small surgical incisions, HSG only requires a small catheter insertion and dye injection. This makes it a preferred first-line diagnostic test for many couples facing infertility.
Understanding the Link Between Infertility and Fallopian Tubes
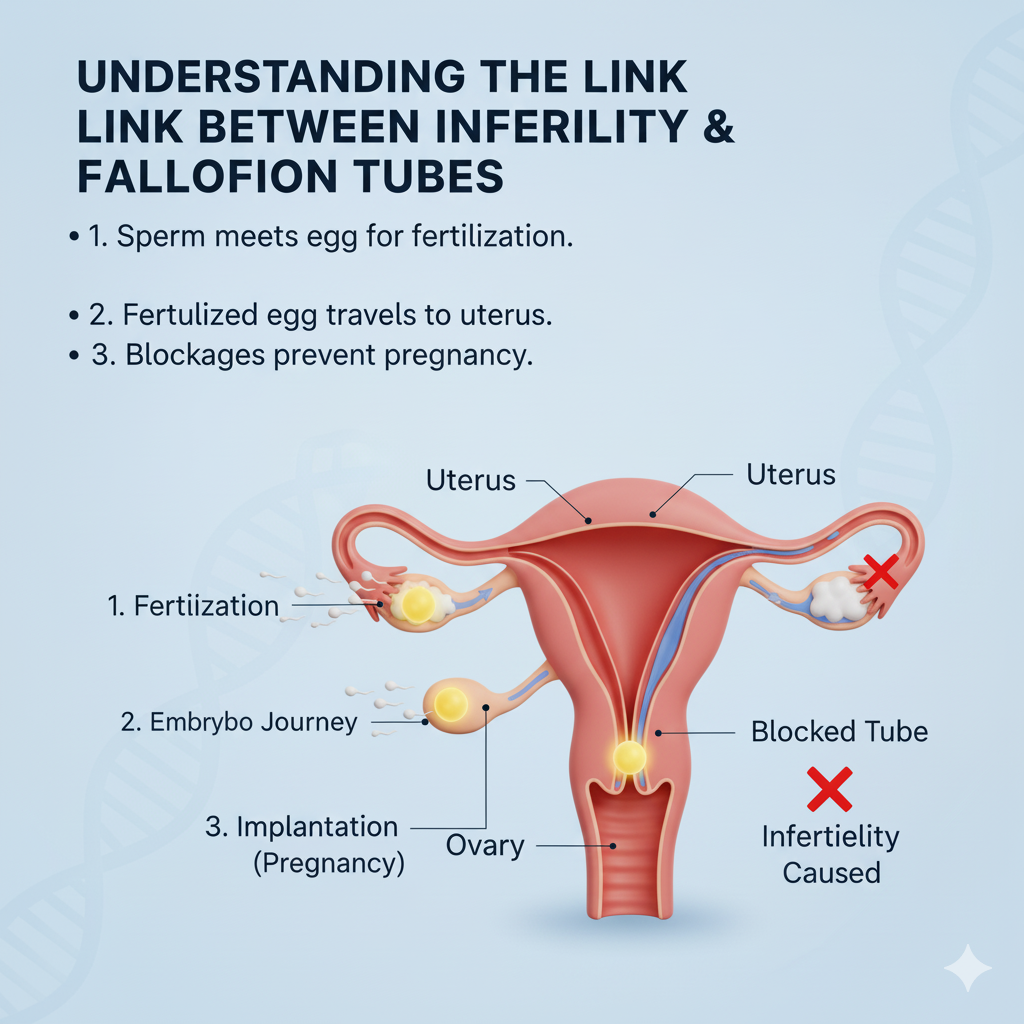
Why Healthy Fallopian Tubes Are Crucial for Conception
The fallopian tubes are the bridges between the ovaries and the uterus. After ovulation, the egg travels from the ovary into the tube, where it meets the sperm for fertilization. Once fertilized, the embryo continues its journey to the uterus for implantation. If either tube is blocked or damaged, the entire process is disrupted, leading to difficulties in conceiving.
Even if only one tube is blocked, fertility may still be reduced because the chances of the egg and sperm meeting become lower. This is why doctors emphasize testing the tubes early in the infertility journey. Without open and functional tubes, even the healthiest eggs and sperm cannot result in pregnancy.
Common Causes of Blocked Fallopian Tubes
Fallopian tube blockages can occur for a variety of reasons, many of which are linked to past infections or untreated medical conditions. The most common causes include:
- Pelvic Inflammatory Disease (PID): Often caused by untreated sexually transmitted infections, leading to scarring inside the tubes.
- Endometriosis: This condition can cause tissue growth around or inside the tubes, blocking the passage of eggs.
- Previous Surgeries: Pelvic or abdominal surgeries can sometimes lead to adhesions or scar tissue that narrows the tubes.
- Tuberculosis (in some regions): Genital TB is a silent cause of infertility in women, often damaging the tubes.
Understanding these causes helps couples see why the HSG test is crucial—it can reveal hidden damage that may not show up in routine scans.
Symptoms That Indicate Tubal Issues
Interestingly, most women with blocked fallopian tubes do not experience obvious symptoms. Infertility itself is often the first sign that something may be wrong. However, some subtle signs might include:
- Chronic pelvic pain
- Painful periods or intercourse
- Abnormal vaginal discharge
- A history of pelvic infections or surgeries
Because these symptoms can easily be mistaken for other conditions, many women remain unaware of tubal issues until they attempt conception. That’s why an HSG test becomes essential—it uncovers problems that may otherwise stay hidden.
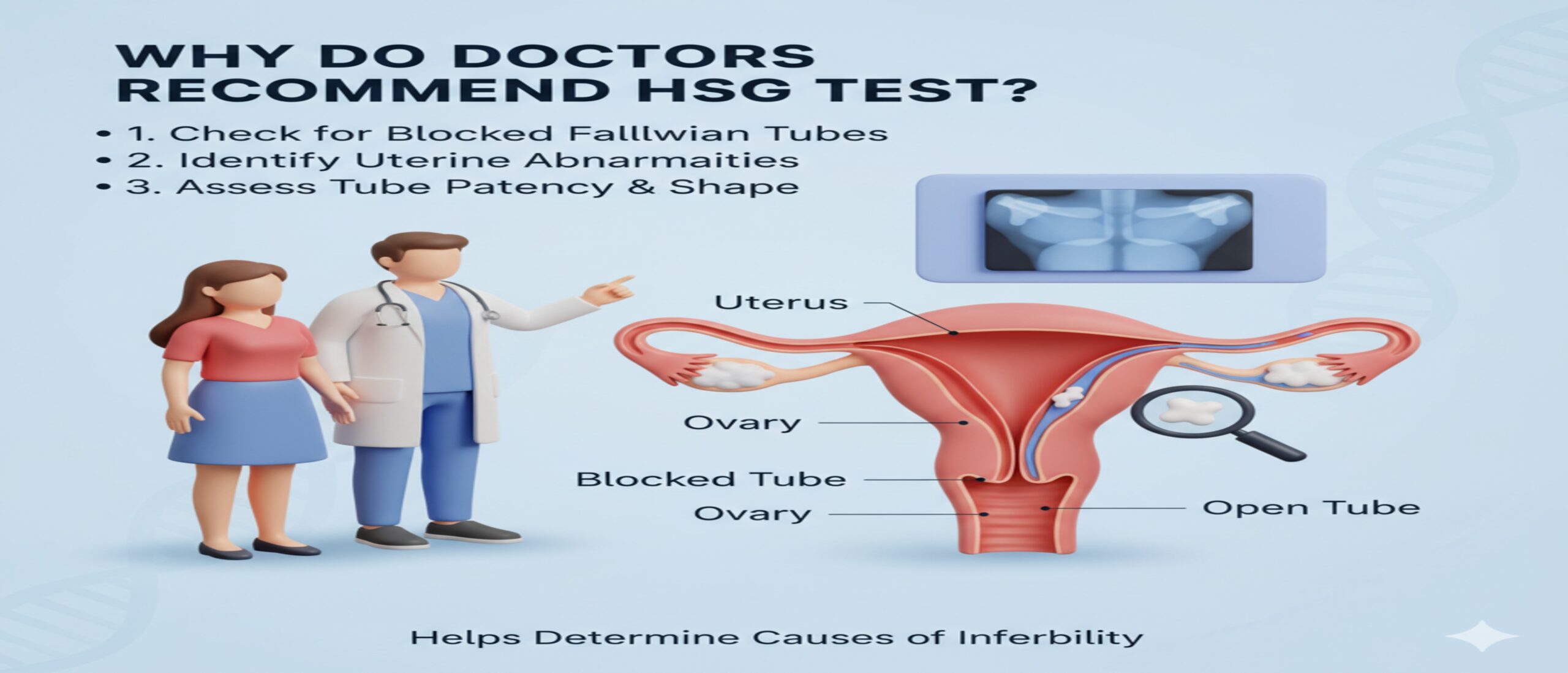
Key Reasons Why Doctors Recommend HSG Test
Detecting Blockages in the Fallopian Tubes
The primary reason doctors recommend an HSG test is to detect whether the fallopian tubes are blocked. If the contrast dye injected during the procedure fails to flow freely through the tubes and into the abdominal cavity, it indicates a blockage. This information is crucial because it helps doctors decide the next steps. For example:
- If the blockage is partial, fertility treatments like IUI may still be possible.
- If both tubes are completely blocked, doctors may recommend IVF, bypassing the need for tubes altogether.
By identifying the exact location and extent of the blockage, the HSG test provides a clear picture for tailored treatment planning.
Evaluating the Shape and Structure of the Uterus
Apart from the tubes, the HSG test also gives a detailed look at the uterine cavity. A healthy uterus should have a triangular shape with no obstructions inside. However, some women may have congenital abnormalities like a bicornuate uterus (heart-shaped) or septate uterus (with a dividing wall). These irregularities can make it harder to conceive or carry a pregnancy to term.
Through HSG imaging, doctors can see if the uterus is structurally normal or if interventions like surgery are needed. Identifying these issues early can save couples from repeated pregnancy losses and failed treatments.
Identifying Uterine Abnormalities that Hinder Pregnancy
Conditions such as fibroids, adhesions, and polyps are common uterine abnormalities that can prevent pregnancy. These growths or scar tissues may block the uterine cavity, preventing the embryo from implanting. The HSG test highlights such irregularities, allowing doctors to plan corrective measures like hysteroscopy or minor surgeries before beginning fertility treatments.
By ruling out these factors, the chances of successful conception—either naturally or through medical assistance—increase significantly.
Assessing Fertility Before IVF or IUI Treatments
Before suggesting expensive treatments like IVF or IUI, doctors want to ensure that the uterus and tubes are healthy enough to support conception. Performing an HSG test before these procedures prevents unnecessary financial and emotional strain. If an abnormality is detected, it can be treated first, thereby improving the success rates of advanced fertility treatments.
Detecting Adhesions, Fibroids, and Polyps
Scar tissues (adhesions), benign growths (fibroids), and small tissue masses (polyps) are often silent obstacles in fertility. The HSG test helps visualize these abnormalities clearly. By knowing whether such conditions exist, doctors can perform corrective procedures, improving the uterine environment for pregnancy.
How the HSG Test is Performed
Step-by-Step Procedure of an HSG Test
The HSG test may sound intimidating, but the procedure is relatively simple and quick. Here’s how it typically goes:
- The test is usually scheduled after menstruation but before ovulation (between day 7–10 of the cycle) to avoid disturbing a potential early pregnancy.
- The patient lies on an X-ray at home, similar to a pelvic exam position.
- A speculum is inserted into the vagina, and a small catheter is placed into the cervix.
- A contrast dye is gently injected into the uterus and fallopian tubes.
- X-ray images are taken as the dye flows through the reproductive system.
- Once the images are captured, the instruments are removed, and the procedure ends.
The entire process usually takes 15–30 minutes, making it one of the most efficient infertility diagnostic tests available.
Duration and Preparation Required for the Test
Preparation for the HSG test is minimal but important. Doctors may prescribe a mild pain reliever or antibiotics to reduce discomfort and prevent infection. Women are advised not to have unprotected intercourse before the test, as it must not be performed if pregnancy is suspected.
The test itself is short, and patients can usually resume normal activities the same day. Mild cramping or spotting is common but usually subsides within a few hours.
Safety Measures During the HSG Procedure
Although the HSG test is generally safe, medical professionals take necessary precautions, including:
- Using sterile equipment to prevent infections
- Administering antibiotics if there’s a higher risk of pelvic infection
- Monitoring for allergic reactions to the dye (which are very rare)
Because the radiation exposure is extremely low, the test is considered safe and does not affect future fertility.
Benefits of HSG Test for Infertility Evaluation
Early Detection of Reproductive Issues
One of the most valuable benefits of the HSG test is its ability to detect reproductive issues early in the infertility journey. Many couples spend years trying to conceive without realizing that the underlying problem is a structural blockage or abnormality. By undergoing an HSG test, couples get a clearer picture of their reproductive health at the very beginning of their fertility evaluation.
For example, if the test shows a blocked fallopian tube, doctors can immediately guide the couple toward IVF, saving them from wasted months of trying naturally. Similarly, if the uterus shows an abnormal shape or growths, corrective procedures can be planned before pregnancy attempts. This proactive approach shortens the infertility journey, reducing emotional stress and improving overall success rates.
Helping Couples Save Time in Infertility Journey
Infertility testing can often feel like a long and uncertain road. Couples may undergo multiple blood tests, ultrasounds, and hormonal evaluations, only to remain without clear answers. The HSG test speeds up this process by providing immediate, visual proof of whether the reproductive pathways are functioning properly.
For instance, instead of waiting several cycles to see if natural conception works, couples with blocked tubes identified through HSG can directly move toward advanced fertility treatments. This time-saving factor is especially critical for women above the age of 35, where fertility naturally declines each year. By cutting down guesswork, HSG allows doctors to design a more targeted and effective fertility plan.
Improves Chances of Choosing the Right Treatment Plan
Every couple’s infertility journey is unique, and what works for one pair may not work for another. The HSG test helps doctors personalize treatment plans based on the exact findings. For example:
- If one tube is open, doctors may suggest timed intercourse or IUI.
- If both tubes are blocked, IVF becomes the recommended option.
- If uterine fibroids are found, a minor surgery may be done before attempting conception.
Without HSG, couples might go through multiple failed cycles of treatment simply because the root problem wasn’t identified. By revealing the real barriers, the HSG test ensures the treatment path chosen has higher chances of success.
Cost-Effectiveness of the HSG Test
Another reason why doctors recommend HSG is its cost-effectiveness compared to other infertility evaluations. While procedures like laparoscopy can be expensive and require hospitalization, HSG is typically performed on an outpatient basis at a lower cost. Considering the valuable information it provides, the test often saves couples money in the long run by preventing unnecessary treatments and guiding them straight to the right fertility solution.
For couples investing in expensive treatments like IVF, ensuring that the uterus and tubes are healthy beforehand is a wise and economical step. Thus, the HSG test is not just medically beneficial but also financially practical.
Possible Risks and Side Effects of HSG Test
Common Discomforts During the Procedure
Like most medical procedures, the HSG test may cause some temporary discomfort. The most common sensations reported include:
- Mild to moderate cramping during dye injection
- Pressure in the lower abdomen
- Slight pain similar to menstrual cramps
These symptoms are short-lived and usually disappear within a few hours after the test. Doctors often recommend taking a mild pain reliever beforehand to minimize discomfort. Some women may also experience light spotting for a day or two, which is considered normal.
Rare Complications After an HSG Test
Although the test is generally safe, there are rare instances where complications can arise. These may include:
- Infection: In very rare cases, bacteria may enter the uterus during the procedure, leading to pelvic infection.
- Allergic Reaction: Some women may be allergic to the contrast dye, though this is uncommon.
- Uterine Injury: Extremely rare, but slight risk exists when inserting instruments into the cervix.
Doctors take precautions to minimize these risks, such as prescribing antibiotics for women with a history of pelvic infections. Overall, the benefits of the test far outweigh the rare possibilities of complications.
Who Should Avoid the HSG Test?
While HSG is highly recommended, not everyone is an ideal candidate. Women should avoid the test if they:
- Are currently pregnant or suspect pregnancy
- Have untreated pelvic infections
- Are allergic to iodine-based contrast dyes
- Have heavy menstrual bleeding at the time of testing
Doctors always review medical history and current health conditions before scheduling the procedure, ensuring it is both safe and effective for each patient.
Alternatives to HSG Test in Infertility Diagnosis
Sonohysterography vs HSG Test
Sonohysterography is an ultrasound-based procedure where saline is injected into the uterus to check for abnormalities. While it provides a good view of the uterine cavity, it cannot evaluate the fallopian tubes as effectively as HSG. This makes HSG the superior choice for couples where tubal blockages are suspected. However, sonohysterography can be a good alternative for women primarily concerned with uterine health.
Hysteroscopy as an Alternative
Hysteroscopy is another diagnostic tool that allows doctors to look directly inside the uterus using a tiny camera. Unlike HSG, it does not use X-rays but provides a clear, real-time view of the uterine lining. This makes it especially useful for diagnosing polyps, adhesions, or fibroids. However, hysteroscopy does not assess tubal health, so it is often performed as a complementary test rather than a substitute.
Laparoscopy vs HSG for Fallopian Tube Blockage
Laparoscopy is a surgical procedure performed under anesthesia where a small camera is inserted into the abdomen to check reproductive organs. It provides the most accurate diagnosis of tubal conditions, including endometriosis. However, due to its invasive nature, it is usually recommended only when other tests (like HSG) suggest abnormalities.
Thus, while laparoscopy is highly detailed, HSG remains the preferred first-line test due to its simplicity, safety, and affordability.
When Should Couples Consider an HSG Test?
Recommended Timeline for Women Under 35
For women under 35, doctors usually recommend trying to conceive naturally for at least 12 months before starting infertility tests. However, if conception doesn’t occur after this period, an HSG test is often one of the first investigations suggested. Since younger women generally have better ovarian reserves, early detection of tubal or uterine issues can significantly improve treatment outcomes.
When to Opt for HSG After Failed Conception Attempts
For women over 35, the recommendation changes slightly. Due to declining fertility with age, doctors suggest starting infertility evaluations after just 6 months of unsuccessful attempts. In these cases, the HSG test is crucial for quickly ruling out tubal blockages or uterine abnormalities. Early intervention prevents unnecessary delays and increases the chances of successful conception.
Role of HSG Test Before Advanced Fertility Treatments
Before proceeding with IVF or IUI, most fertility specialists require an HSG test to ensure that the uterus and fallopian tubes are healthy. Attempting advanced treatments without confirming reproductive tract health can lead to repeated failures and wasted resources. By performing HSG beforehand, doctors can plan the treatment more strategically, thereby improving success rates.
Emotional Impact of Infertility Testing on Couples
Coping with Anxiety Before the HSG Test
For many women, the idea of undergoing an HSG test can bring feelings of nervousness or fear. The thought of discomfort during the procedure, combined with the uncertainty of the results, may trigger anxiety. This is completely natural—after all, the test holds significant weight in determining the future path of a couple’s fertility journey.
To manage these feelings, preparation is key. Understanding the procedure beforehand helps reduce fear of the unknown. Many women find it helpful to talk with their doctor about pain management options or even read stories of others who have undergone the test. Relaxation techniques such as deep breathing, meditation, or listening to calming music before the test can also ease anxiety. Couples should remind themselves that the HSG test is not just another medical exam—it is a powerful tool that may bring them one step closer to their dream of parenthood.
Supporting Your Partner Through Infertility Tests
Infertility affects both partners, even though many of the tests focus on the woman’s reproductive system. The emotional weight of an HSG test can feel overwhelming if faced alone, which is why partner support is so important. Men can show support by accompanying their partners to the clinic, offering reassurance, and being available to discuss concerns before and after the procedure.
Simple gestures such as holding hands during the wait, preparing a comfortable space at home for recovery, or even celebrating the courage it takes to undergo the test can make a huge difference. Infertility challenges often strain relationships, but going through these tests as a team can strengthen emotional bonds and provide much-needed comfort during stressful times.
Importance of Counseling During Fertility Diagnosis
The emotional journey of infertility often goes beyond physical health. Couples may experience frustration, sadness, or even guilt when test results reveal obstacles to conception. This is where counseling plays a vital role. Fertility counselors or therapists can help couples process emotions, reduce stress, and build coping strategies for difficult moments.
By openly discussing fears, expectations, and feelings of disappointment, couples can prevent emotional distress from turning into long-term strain. Counseling also provides tools to stay positive and hopeful, even when the fertility journey feels long and uncertain. For many couples, emotional well-being is just as important as medical treatment in achieving success.
Lifestyle Factors That Influence Fertility and HSG Results
Diet and Nutrition for Reproductive Health
Nutrition plays a significant role in fertility and overall reproductive health. A diet rich in vitamins, minerals, and antioxidants can improve egg quality, sperm health, and hormonal balance. Women preparing for an HSG test or fertility treatments are often encouraged to eat foods that support reproductive wellness, such as:
- Leafy greens rich in folic acid
- Whole grains for stable blood sugar levels
- Lean proteins like fish, chicken, and beans
- Nuts and seeds for omega-3 fatty acids
On the other hand, excessive caffeine, alcohol, and processed foods may negatively impact fertility. Maintaining a balanced diet not only supports test results but also increases the chances of successful conception afterward.
Impact of Stress on Fertility and Testing
Stress is often underestimated in discussions about fertility, but it has a powerful influence on reproductive health. Chronic stress can affect hormone regulation, leading to irregular menstrual cycles, delayed ovulation, or reduced sperm quality in men. High stress levels can also make medical procedures, including the HSG test, feel more painful or emotionally draining.
Incorporating stress management techniques—such as yoga, meditation, or journaling—can improve both emotional well-being and physical readiness for fertility testing. By reducing anxiety, couples also create a more positive environment for conception to occur.
Exercise, Weight, and Hormonal Balance
Maintaining a healthy weight is another critical factor in fertility. Both underweight and overweight conditions can disrupt hormonal balance, leading to irregular ovulation or reduced sperm count. Moderate exercise helps regulate hormones, improves circulation, and supports a healthy body weight.
However, extreme exercise can sometimes do more harm than good, especially for women. Too much physical strain may interfere with ovulation cycles. The key is balance—gentle activities like walking, swimming, or yoga provide health benefits without overstressing the body. When combined with a nutritious diet and emotional care, lifestyle adjustments can complement the benefits of an HSG test and fertility treatments.
Success Stories Linked to HSG Test
Couples Conceiving Naturally After HSG
Interestingly, many couples report conceiving naturally shortly after an HSG test. Some researchers believe that the process of injecting contrast dye may help flush out minor blockages or debris in the fallopian tubes, temporarily increasing fertility. While this effect is not guaranteed, it offers hope to couples who may otherwise feel discouraged.
Stories of women becoming pregnant within months of their HSG test are not uncommon, adding a layer of optimism to the procedure. For couples, this possibility turns the test into not just a diagnostic tool but also a potential fertility booster.
How HSG Helped in Choosing the Right Treatment
For other couples, the HSG test becomes a turning point in their fertility journey. For example, some discover that both tubes are blocked, leading doctors to recommend IVF as the best option. Others may learn about fibroids or polyps that can be surgically corrected. In these cases, the HSG test provides clarity and direction, sparing couples from months of ineffective treatments.
By giving precise answers, HSG removes uncertainty and allows couples to focus on treatments with the highest chance of success. Many couples describe this clarity as life-changing, as it restores hope and confidence in their path toward parenthood.
Role of HSG in Assisted Reproductive Success
For couples pursuing advanced treatments such as IVF or IUI, the HSG test plays a crucial role in maximizing success rates. Knowing that the uterus is free from abnormalities ensures that embryos have the best possible environment for implantation. Similarly, confirming tubal health allows doctors to select the most appropriate procedure.
Couples who undergo HSG before assisted reproductive technologies often report fewer failed cycles and greater peace of mind. This highlights the test’s importance not just as a diagnostic tool but as a strategic step in fertility planning.
Frequently Asked Questions About HSG Test
Is the HSG Test Painful?
Discomfort levels vary from woman to woman. Some describe it as mild cramping similar to period pain, while others feel stronger cramps during the dye injection. The discomfort usually lasts only a few minutes and subsides quickly after the procedure. Pain relievers taken before the test can help make the experience easier.
Can You Get Pregnant Immediately After HSG?
Yes, some women do conceive soon after an HSG test, possibly due to the clearing effect of the dye on minor blockages. While it is not a guaranteed outcome, many doctors advise couples to try naturally in the months following the test, as fertility may be temporarily enhanced.
How Soon Are Results Available?
The results of an HSG test are often available immediately, as the X-ray images are taken in real time. The radiologist or fertility specialist can explain whether the tubes are open and if the uterus appears normal. This instant feedback allows couples to discuss next steps with their doctor without long waiting periods.
Myths and Misconceptions About HSG Test
Misbeliefs About Radiation Exposure
One of the most common myths surrounding the HSG test is the fear of excessive radiation. Many women worry that since X-rays are used, the radiation might harm their reproductive organs or reduce fertility. In reality, the amount of radiation used in an HSG test is extremely low and considered safe. It is carefully regulated to ensure no long-term risks. The exposure is often compared to that of a routine dental X-ray—minimal and harmless.
Doctors also schedule the test in the first half of the menstrual cycle to avoid performing it during early pregnancy, further ensuring safety. Women should rest assured that radiation is not a reason to avoid HSG and that the benefits far outweigh the negligible exposure.
Myths About Infertility Causes
Another common misconception is that infertility is always due to the woman’s reproductive system. Many couples believe that the HSG test will provide all the answers and that once the tubes and uterus are checked, the issue is solved. However, infertility is often a shared condition, with male factors such as low sperm count or poor motility contributing to nearly 40% of cases.
The HSG test is an important tool, but it is only part of a comprehensive fertility evaluation. Both partners should undergo testing to identify all possible contributing factors. Correcting this myth is essential to avoid placing undue emotional burden on women alone.
Clarifying Concerns About Test Accuracy
Some couples doubt whether the HSG test is truly accurate. While no test is 100% perfect, HSG is considered highly reliable in detecting blockages, uterine abnormalities, and structural concerns. False positives can occur in rare cases, particularly if muscle spasms temporarily block the tube during the test. However, doctors are trained to interpret these situations carefully, sometimes recommending follow-up evaluations like laparoscopy if needed.
The misconception that HSG is “unreliable” often comes from misunderstandings or outdated experiences. Today’s modern techniques and advanced imaging make the HSG test one of the most dependable first-line infertility investigations.
Conclusion
The HSG test (hysterosalpingography) is far more than a routine medical procedure—it is a key diagnostic step for couples struggling with infertility. By providing clear insights into the health of the fallopian tubes and uterus, it helps doctors uncover hidden obstacles that prevent conception. Whether it’s detecting blockages, identifying uterine abnormalities, or ensuring readiness for treatments like IVF or IUI, the HSG test saves time, money, and emotional strain.
Beyond its diagnostic value, the HSG test often brings unexpected blessings, with many couples reporting natural conception soon after the procedure. While it may involve mild discomfort, the test is safe, effective, and often life-changing for those on the path to parenthood.
For couples facing infertility, undergoing an HSG test is not just about getting answers—it is about taking a proactive step toward hope, clarity, and the possibility of building the family they have long dreamed of.
5 Unique FAQs About HSG Test
- Can HSG test results change over time?
Yes, results may change. For example, if a tube is clear during one test, it could become blocked later due to new adhesions or infections. This is why some women may need repeat evaluations if conception does not occur after several months. - Does the HSG test require anesthesia?
No, anesthesia is not required. The test is typically performed while the patient is awake. Mild painkillers may be recommended, but the procedure is brief and does not involve surgery. - How long should couples wait to try conceiving after HSG?
Couples can often try as soon as the next cycle. In fact, many doctors encourage attempting conception right away since fertility may be temporarily enhanced after the test. - Can men benefit from HSG test results?
Indirectly, yes. While the test evaluates the woman’s reproductive system, it also helps men by clarifying whether infertility is due to tubal or uterine issues. This guides both partners toward a more accurate treatment plan.
5. Is the HSG test recommended for women with recurrent miscarriages?
Yes, doctors often recommend HSG for women who experience repeated pregnancy losses. The test can reveal uterine abnormalities, adhesions, or structural issues that may interfere with successful implantation and pregnancy.

Leave a Reply