Introduction to Chikungunya Virus
What is Chikungunya?
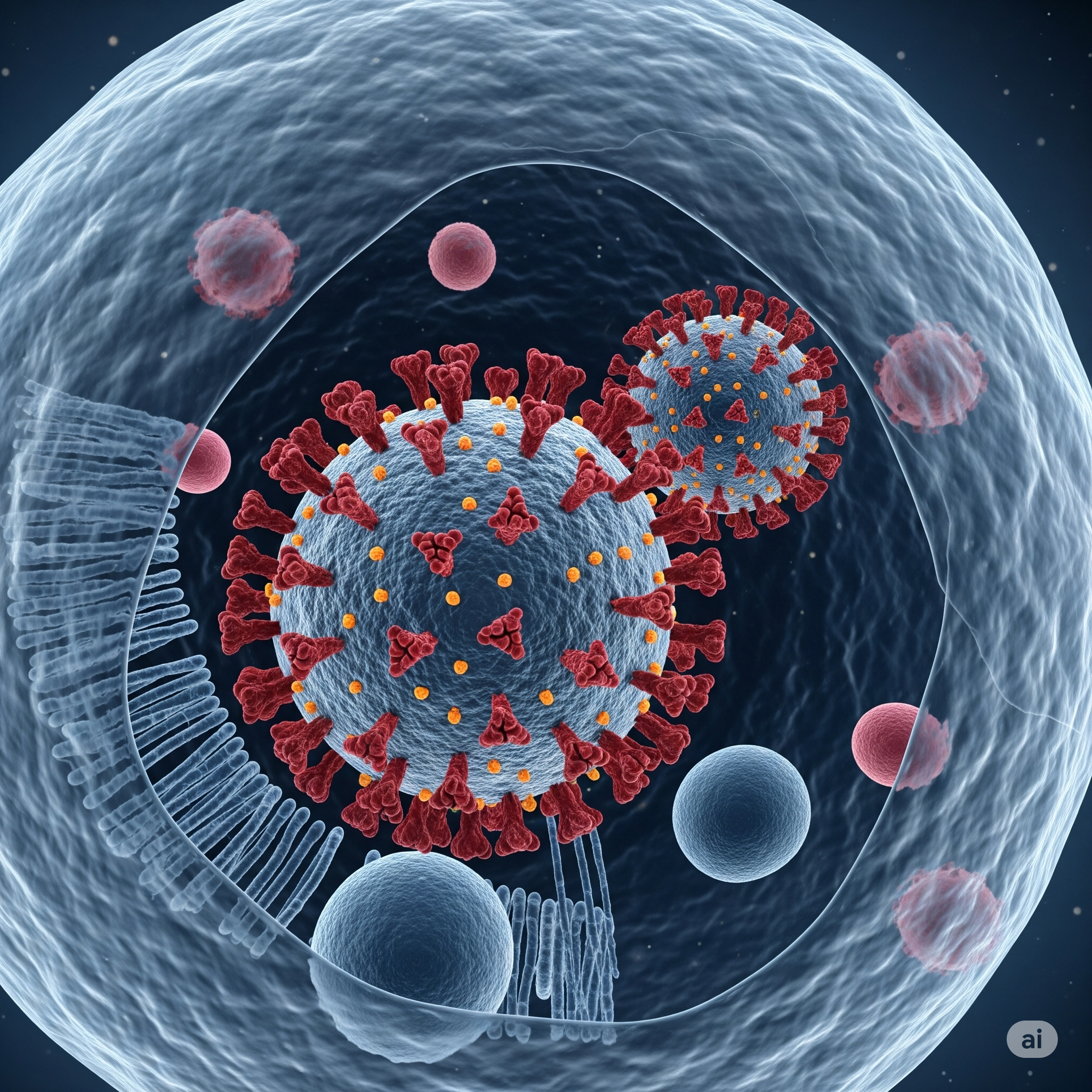
Chikungunya is a mosquito-borne viral disease that causes fever and severe joint pain. The name “Chikungunya” originates from the Makonde language, meaning “to become contorted,” referring to the stooped posture of sufferers due to intense joint pain. Caused by the Chikungunya virus (CHIKV), this illness can also produce symptoms like muscle pain, rash, fatigue, and headache. Although it’s rarely fatal, the pain can be debilitating and persist for weeks, months, or even longer.
The virus belongs to the Alphavirus genus of the Togaviridae family. After the bite of an infected mosquito, symptoms typically begin 4–8 days later, but they can start anywhere between 2 to 12 days. Unlike some other mosquito-borne diseases, Chikungunya doesn’t usually result in severe complications, but it can greatly affect quality of life, particularly among older adults or those with existing health conditions.
History and Global Spread of Chikungunya
Chikungunya was first identified during an outbreak in southern Tanzania in 1952. Initially considered an African disease, it has since spread across Asia, Europe, and the Americas due to increased global travel, urbanization, and climate change. Significant outbreaks have occurred in India, the Caribbean, and parts of South and Central America.
The spread of Aedes aegypti and Aedes albopictus mosquitoes—both capable of transmitting the virus—has facilitated the geographical expansion of Chikungunya. Regions that were once unaffected have now become vulnerable due to warming temperatures and changing rainfall patterns, which create ideal breeding grounds for these mosquitoes.
In the past decade, global health authorities have noted a surge in Chikungunya cases. Local health systems in affected areas often struggle to manage outbreaks due to overwhelmed infrastructure and lack of awareness. As a result, the virus has become a significant public health concern in tropical and subtropical regions.
Causes of Chikungunya Infection
Primary Chikungunya Virus Transmission
Chikungunya is primarily spread to humans through the bite of an infected female mosquito. The two main culprits are Aedes aegypti and Aedes albopictus. These mosquitoes are aggressive daytime biters, with peak activity in the early morning and late afternoon. Once a mosquito feeds on a person infected with the Chikungunya virus, it becomes a carrier within 4–7 days and can then transmit the virus to other individuals it bites.
The virus cannot be transmitted from human to human through casual contact, coughing, or sneezing. However, rare cases of transmission through blood transfusions, organ transplants, or from mother to newborn during childbirth have been reported. These cases are exceptionally uncommon but highlight the need for comprehensive monitoring.
In areas with ongoing outbreaks, it’s common for multiple people in the same household or community to be affected due to the rapid breeding and feeding cycles of mosquitoes. That’s why controlling mosquito populations is critical to preventing transmission.
Role of Mosquito Vectors in Spreading Chikungunya
The Aedes mosquitoes are highly adaptive, thriving in both urban and rural environments. Aedes aegypti typically breeds in clean, stagnant water sources found in artificial containers like flower pots, tires, and water storage tanks. Aedes albopictus, also known as the Asian tiger mosquito, is capable of surviving in cooler climates and has spread widely due to international trade and climate adaptability.
These mosquitoes lay eggs in dry conditions and can survive for months. Once in contact with water, the eggs hatch and mature into adult mosquitoes within a week, leading to explosive population growth. This makes even a small water source a potential breeding ground and underlines the importance of consistent sanitation and monitoring.
The short development cycle and aggressive biting habits of Aedes mosquitoes allow the virus to spread rapidly in densely populated areas. Public awareness about the breeding habits of these vectors is essential in controlling outbreaks.
Environmental and Seasonal Risk Factors
Environmental factors play a major role in Chikungunya outbreaks. Rainy seasons create ideal conditions for mosquito breeding, especially in regions lacking adequate drainage or waste management systems. Areas with poor sanitation, stagnant water, and high population density are particularly vulnerable.
In many tropical countries, the rise in temperature during certain months accelerates mosquito reproduction. This, combined with increased travel and limited mosquito control efforts, can turn a localized infection into a full-blown epidemic.
Climate change has also altered the geographic range of Aedes mosquitoes. Warmer temperatures and irregular rainfall patterns have expanded mosquito habitats to higher altitudes and latitudes, exposing new populations to Chikungunya for the first time. These changes necessitate a more proactive approach to environmental management and vector control.
Key Symptoms of Chikungunya Virus
Early Symptoms of Chikungunya
Chikungunya symptoms usually appear 2–12 days after being bitten by an infected mosquito. The most recognizable signs are sudden-onset high fever and severe joint pain. This joint pain is typically bilateral and affects the hands, feet, wrists, and ankles. The discomfort can be so intense that it hinders movement and daily activities.
Other early symptoms include:
- Headache
- Muscle pain
- Fatigue
- Rash (usually appearing 2–5 days after fever)
- Swelling in joints
In some cases, conjunctivitis, nausea, vomiting, and abdominal pain may also occur. These symptoms generally last from a few days to a week. However, in older adults or those with underlying conditions, symptoms can persist longer and may lead to complications.
Unlike the flu or common cold, Chikungunya fever comes on suddenly and is often accompanied by incapacitating joint pain, making it easier to distinguish in endemic areas. Rapid diagnosis and symptom management are crucial during this stage to ensure proper care.
Chronic Symptoms and Long-Term Effects
For most people, the acute phase resolves within a week, but others—especially older adults—may experience chronic joint pain for months or even years. This post-viral arthritis resembles rheumatoid arthritis and can be both physically and emotionally draining.
Chronic symptoms include:
- Persistent joint inflammation
- Stiffness and swelling
- Muscle weakness
- Difficulty walking or performing daily tasks
These prolonged effects are not well understood but are thought to be due to the virus triggering an autoimmune response in the body. Physical therapy, anti-inflammatory medications, and lifestyle adjustments may be required to manage these symptoms.
In rare instances, neurological complications such as encephalitis, meningoencephalitis, or Guillain-Barré syndrome can occur. These are more likely in infants, the elderly, and those with weakened immune systems.
Differences Between Chikungunya, Dengue, and Zika
Chikungunya is often mistaken for dengue or Zika because they share similar symptoms and are transmitted by the same mosquitoes. However, there are distinct differences:
- Chikungunya causes intense joint pain and rash, but rarely bleeding or shock.
- Dengue can lead to severe bleeding, low platelet count, and in extreme cases, dengue hemorrhagic fever.
- Zika is usually mild but is associated with birth defects like microcephaly when contracted during pregnancy.
Correct diagnosis is essential to determine the right course of treatment, especially during simultaneous outbreaks where multiple viruses may be present in the same region.
Chikungunya Diagnosis and Testing
How Doctors Diagnose Chikungunya
Diagnosing Chikungunya isn’t always straightforward, especially in areas where dengue and Zika are also common. Since these mosquito-borne illnesses have overlapping symptoms, doctors must rely on a combination of clinical signs, patient history, and lab tests. Diagnosis often begins with an evaluation of symptoms such as sudden high fever, intense joint pain, rash, and fatigue—particularly if the patient has recently traveled to or resides in an endemic area.
During the acute phase, healthcare providers typically look for hallmark features like symmetrical joint swelling and rash patterns. A patient’s travel history is especially important. If they’ve been to a tropical or subtropical region recently, the likelihood of a mosquito-borne infection increases. Physicians may also ask about recent mosquito bites, exposure to stagnant water, and others in the household being sick.
It’s important for healthcare workers to rule out dengue first because it can be life-threatening, especially if mismanaged. Dengue and Chikungunya can coexist in the same area, and co-infection is possible. While clinical evaluation gives a good indication, laboratory testing remains the gold standard for a confirmed diagnosis.
Common Laboratory Tests for Chikungunya
Several tests help confirm a Chikungunya infection. During the first few days of symptoms, when the virus is present in the bloodstream, doctors often order a reverse transcription-polymerase chain reaction (RT-PCR) test. This highly sensitive method detects viral RNA and confirms the infection quickly and accurately.
Another key diagnostic method is serological testing, which involves detecting specific antibodies—IgM and IgG—in the blood. IgM antibodies are usually detectable about 4–5 days after symptom onset and can remain present for several weeks. IgG antibodies appear later and indicate past exposure.
Here are the most commonly used lab tests for Chikungunya:
- RT-PCR Test: Detects viral RNA in blood.
- ELISA Test: Detects IgM and IgG antibodies.
- Virus Isolation: Culturing the virus in a lab (rarely done due to complexity).
A CBC test might also be done to rule out dengue, especially if platelet levels are normal. Since Chikungunya rarely causes low platelet counts, it helps distinguish it from dengue fever.
Challenges in Identifying Chikungunya
Identifying Chikungunya in the early stages can be difficult, particularly in regions where multiple arboviruses are endemic. This diagnostic confusion often leads to delays in treatment or misdiagnosis. Since many cases occur in resource-limited settings, access to advanced laboratory tests may be restricted.
One of the biggest challenges is the similarity between Chikungunya and dengue, both in symptoms and timing. Misdiagnosis can result in unnecessary hospitalization or incorrect medication, such as administering NSAIDs in suspected dengue cases, which can increase the risk of bleeding.
Moreover, patients with chronic joint pain due to past infections may be misdiagnosed with other autoimmune conditions like rheumatoid arthritis. A lack of awareness among healthcare workers and patients further complicates timely diagnosis.
In outbreak scenarios, the surge in patient volume can overwhelm diagnostic labs. This highlights the need for rapid point-of-care tests and better surveillance systems. Community health education can also play a vital role in early recognition and reporting of symptoms.
Treatment and Management of Chikungunya
Medical Treatment Options for Chikungunya
Currently, there is no specific antiviral treatment for Chikungunya. Instead, treatment focuses on relieving symptoms, especially joint pain and fever. Most patients recover completely within a few weeks, but supportive care is essential to manage discomfort and avoid complications.
Common medical treatments include:
- Acetaminophen (Paracetamol) for fever and pain.
- Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (only if dengue is ruled out).
- Hydration therapy to replace lost fluids from fever and sweating.
- Rest to allow the body to heal naturally.
Severe joint pain may require corticosteroids or other anti-inflammatory medications under medical supervision. Patients with pre-existing joint issues, such as osteoarthritis, may experience worsened symptoms and need additional rheumatologic care.
Hospitalization is rare but may be required for elderly patients, infants, or those with comorbidities like diabetes or cardiovascular issues. In such cases, close monitoring for complications such as dehydration, hypotension, or secondary infections is crucial.
Self-medication is discouraged, especially without knowing whether the infection is Chikungunya or dengue. Always consult a healthcare professional for the correct diagnosis and treatment plan.
Home Remedies and Natural Relief
In addition to medical treatment, many people seek natural ways to relieve Chikungunya symptoms. While these remedies don’t cure the disease, they can help ease joint discomfort, boost immunity, and promote recovery.
Some effective home remedies include:
- Turmeric and Milk: The anti-inflammatory properties of turmeric may help reduce joint swelling and pain.
- Ginger Tea: Acts as a natural anti-inflammatory agent.
- Neem Leaves: Known for their antiviral and antibacterial properties; can be used in baths or teas.
- Tulsi (Holy Basil): Helps with fever reduction and supports the immune system.
- Papaya Leaf Juice: Commonly used in dengue, but also considered beneficial in maintaining platelet levels.
Additionally, applying warm compresses to painful joints and engaging in gentle stretching exercises can alleviate stiffness. However, strenuous activity should be avoided during the acute phase of illness.
Adequate rest, hydration, and a balanced diet rich in fruits, vegetables, and lean proteins also play a significant role in speeding up recovery. It’s important to avoid alcohol and processed foods, which can hinder the immune response.
Long-Term Care for Chronic Joint Pain
Chronic joint pain following Chikungunya can persist for months or even years, particularly among older adults or those with pre-existing joint conditions. This phase resembles post-viral arthritis and requires consistent management to maintain quality of life.
Long-term strategies include:
- Regular Physical Therapy: Helps maintain joint flexibility and strength.
- Anti-inflammatory Medications: May be prescribed for extended periods under medical supervision.
- Low-Impact Exercise: Activities like yoga, swimming, or tai chi can be beneficial without putting too much stress on the joints.
- Dietary Changes: Incorporating anti-inflammatory foods such as omega-3-rich fish, leafy greens, berries, and turmeric can help manage symptoms.
Patients are often advised to monitor joint pain levels and keep a symptom diary to share with their healthcare provider. This allows for a more personalized treatment plan and timely adjustment of therapies.
Mental health is also a crucial aspect of long-term care. Chronic pain can lead to anxiety, depression, or social withdrawal. Support groups, counseling, and mindfulness practices can improve emotional well-being.
Preventing Chikungunya Infection
Mosquito Bite Prevention Techniques
Preventing mosquito bites is the first and most effective line of defense against Chikungunya. Since there is no specific antiviral treatment or widely available vaccine, individual actions play a crucial role in reducing infection risk. Understanding mosquito behavior is essential—Aedes mosquitoes are most active during daylight hours, particularly during early morning and late afternoon.
Here are the top strategies for mosquito bite prevention:
- Wear Protective Clothing: Cover as much skin as possible. Long-sleeved shirts, long pants, socks, and closed-toe shoes are effective barriers.
- Use Mosquito Repellent: Products containing DEET, picaridin, or oil of lemon eucalyptus are recommended. Apply to exposed skin and reapply as directed.
- Install Screens and Nets: Keep windows and doors closed or install screens to prevent mosquitoes from entering living spaces. Use mosquito nets, especially when sleeping during the day.
- Use Insecticides Indoors: Aerosol sprays, mosquito coils, or plug-in vapor repellents can help eliminate mosquitoes inside the home.
- Avoid Scented Products: Mosquitoes are attracted to strong scents, so avoid perfumes and scented lotions when outdoors.
Parents should be especially cautious with young children, using repellent products appropriate for their age and avoiding excessive outdoor exposure during peak mosquito activity times. Travelers to endemic regions should take extra precautions, especially when visiting rural or forested areas.
Environmental Control and Sanitation
Eliminating mosquito breeding grounds is one of the most sustainable methods to control the spread of Chikungunya. Aedes mosquitoes breed in clean, stagnant water, often found in containers around homes and communities.
Key environmental control measures include:
- Empty and Clean Water-Holding Containers: Buckets, flowerpots, birdbaths, and pet water bowls should be emptied and scrubbed weekly to eliminate eggs and larvae.
- Cover Water Storage: Use tight lids or mosquito-proof mesh to cover water tanks and barrels.
- Improve Waste Management: Dispose of discarded tires, plastic containers, and other junk that can collect water.
- Clear Drainage Channels: Blocked drains and gutters can become mosquito breeding havens if left unchecked.
- Introduce Biological Control: In some regions, introducing larvivorous fish to water bodies or using bacterial agents like Bacillus thuringiensis israelensis (Bti) can help control larvae without harming the environment.
Community-level action is essential. One person cleaning their yard isn’t enough if neighbors aren’t doing the same. Collective efforts such as cleanup drives and public awareness campaigns can make a significant difference.
Travel Precautions in Endemic Areas
Travelers visiting Chikungunya-prone regions need to take additional precautions before, during, and after their trip. Whether for tourism, work, or family visits, the risk of contracting the virus is real, especially during the rainy season when mosquito populations surge.
Before travel:
- Check Health Advisories: Refer to travel health notices from reputable health organizations for up-to-date outbreak information.
- Pack Repellents and Mosquito Nets: Make sure to bring your own supply of repellent and portable nets, especially if visiting rural or underdeveloped areas.
- Choose Accommodations Wisely: Opt for air-conditioned rooms with screened windows and doors to reduce mosquito entry.
During travel:
- Stay Covered: Continue wearing protective clothing and applying repellent daily.
- Avoid Outdoor Activities at Peak Hours: Limit time spent outdoors at dawn and dusk when mosquitoes are most active.
- Stay Hydrated and Rested: A strong immune system can better handle viral exposure.
After travel:
- Monitor Symptoms: Watch for fever, joint pain, rash, or fatigue for up to two weeks after returning. Seek medical attention promptly if symptoms arise.
- Avoid Mosquito Exposure at Home: If infected, staying indoors and using mosquito protection can prevent local transmission, especially in areas where Aedes mosquitoes are present.
Impact of Chikungunya on Public Health
Economic and Social Consequences
Chikungunya may not be fatal, but its impact on public health and society is significant. During outbreaks, the burden on healthcare systems escalates rapidly, especially in resource-constrained regions. Clinics and hospitals become overwhelmed with patients suffering from fever, joint pain, and fatigue, straining both manpower and medical supplies.
Economically, Chikungunya leads to lost productivity as infected individuals are unable to work for days or even weeks. This affects families, small businesses, and larger economies. In rural and agricultural communities, the illness can delay harvests, reduce income, and lead to food insecurity. In urban areas, widespread absenteeism affects service delivery and education.
Chronic symptoms that linger for months, particularly joint pain, can result in long-term disability, requiring prolonged treatment, rehabilitation, and financial support. For daily wage earners and informal workers, even a week of illness can mean the difference between survival and hardship.
The cost of prevention programs, awareness campaigns, and medical care also adds to the burden on government budgets. During large outbreaks, emergency funding is often needed for vector control measures, such as fumigation and community sanitation drives.
Chikungunya Outbreaks in Urban Populations
Urban centers are particularly vulnerable to Chikungunya outbreaks due to high population density, poor sanitation, and the abundance of artificial breeding sites. Stagnant water in construction sites, clogged drains, and uncovered containers in households provide ideal conditions for Aedes mosquitoes.
One of the biggest challenges in cities is managing vector control across informal settlements or slums, where infrastructure is inadequate. In these areas, limited access to clean water often leads residents to store water in open containers, further encouraging mosquito breeding.
Outbreaks in urban settings also spread more rapidly because of the close proximity of people and fast movement within cities. Public transportation systems, schools, workplaces, and marketplaces become hotbeds of transmission when infected individuals move around freely.
Inadequate urban planning, especially in rapidly growing cities, adds another layer of complexity. Municipal authorities often lack the resources and coordination required to launch effective mosquito control efforts during emergencies. Additionally, public awareness tends to be low in these settings, making education campaigns essential.
Vulnerable Populations and Risk Groups
While Chikungunya affects people of all ages, some groups are more vulnerable to severe disease and complications. Infants, elderly individuals, pregnant women, and those with pre-existing medical conditions like diabetes or heart disease are at a higher risk.
In infants, the immune system is still developing, which makes them more susceptible to prolonged symptoms and complications. In rare cases, vertical transmission from mother to child can occur during childbirth, particularly if the mother is in the viremic phase.
Older adults tend to suffer from more intense joint pain, which can aggravate existing arthritis or lead to long-term disability. Recovery in this age group is often slower, and the chances of chronic post-viral arthritis are higher.
Pregnant women, although not at risk of severe symptoms themselves in most cases, must be cautious due to the potential risk to the fetus during perinatal transmission.
People with compromised immune systems—such as cancer patients, those on immunosuppressive drugs, or individuals with HIV/AIDS—may experience a more aggressive course of the disease. It is essential for these individuals to avoid mosquito exposure and seek prompt medical attention if symptoms develop.
Chikungunya and Climate Change
How Climate Affects Mosquito-Borne Viruses
Climate change plays a critical role in the growing prevalence of mosquito-borne diseases like Chikungunya. Rising global temperatures, erratic rainfall patterns, and increasing humidity levels all contribute to expanding mosquito habitats and breeding cycles. These environmental shifts allow disease-carrying mosquitoes—especially Aedes aegypti and Aedes albopictus—to thrive in regions previously considered unsuitable.
Warmer climates accelerate mosquito development, reduce the time it takes for Chikungunya virus to incubate inside mosquitoes, and boost biting frequency. As a result, the transmission cycle becomes faster and more intense. For instance, in areas that once experienced seasonal mosquito activity, climate change is turning this into a year-round problem.
Rainfall is another key factor. While heavy rains can flush out mosquito larvae, intermittent and scattered rain creates stagnant water pools—perfect breeding grounds for mosquitoes. Droughts also contribute when people store water in open containers, inadvertently inviting mosquitoes into their homes.
Urbanization combined with climate change is making things worse. Expanding cities often lack adequate drainage and waste management systems, leading to waterlogging and mosquito infestations. All these factors together create a dangerous cocktail, driving a surge in Chikungunya cases globally.
Future Risk Zones for Chikungunya
Traditionally, Chikungunya was restricted to tropical and subtropical regions. However, due to global warming, new geographical zones—especially in Europe, North America, and East Asia—are becoming increasingly vulnerable. With milder winters and extended warm seasons, Aedes mosquitoes are slowly infiltrating temperate zones.
For example, outbreaks have already been recorded in parts of Southern Europe and even the United States. As temperatures rise, these regions may experience more frequent and severe outbreaks unless preventive measures are implemented swiftly.
Predictive models suggest that by 2050, many urban centers across continents could be at high risk of vector-borne diseases due to climate-induced changes. International travel and trade further facilitate the virus’s spread, as travelers can unknowingly carry the virus to non-endemic areas, where Aedes mosquitoes are present and ready to bite.
To tackle this emerging threat, governments must integrate climate data into public health planning. Early warning systems, real-time disease surveillance, and proactive mosquito control campaigns will be essential to mitigate future outbreaks.
Ongoing Research and Vaccine Development
Scientific Advances in Chikungunya Research
Over the past two decades, Chikungunya has transitioned from a neglected tropical disease to a global public health concern. This growing threat has accelerated research efforts to better understand the virus, its transmission dynamics, and long-term impacts on human health.
Researchers are exploring the virus’s genetic structure to identify vulnerabilities that can be targeted through antiviral drugs or vaccines. Studies are underway to understand why some individuals develop chronic joint pain while others recover quickly. Insights from these studies could lead to improved therapies and personalized treatment plans.
Vector biology is another active area of research. Scientists are studying the behavior and genetics of Aedes mosquitoes to develop more effective vector control methods. These include genetically modified mosquitoes, sterile insect techniques, and innovative larvicides that disrupt mosquito reproduction without harming the environment.
Advanced diagnostic tools are also in development. Rapid test kits that provide results in minutes can revolutionize outbreak response, especially in rural or under-resourced areas.
Status of Chikungunya Vaccine Development
The absence of a commercially available vaccine remains one of the biggest challenges in Chikungunya control. However, progress is being made. Several vaccine candidates are currently in different stages of clinical trials, ranging from traditional inactivated vaccines to modern mRNA-based formulas.
Some of these candidates have shown promising results in early-phase trials, providing long-lasting immunity with minimal side effects. Regulatory approvals, large-scale trials, and manufacturing capacity remain hurdles, but optimism is growing in the scientific community.
Until a vaccine becomes widely available, prevention through mosquito control, personal protection, and public education will continue to be the cornerstone of Chikungunya mitigation.
Myths and Misconceptions About Chikungunya
Common Myths Debunked
Misinformation spreads almost as fast as viruses. During Chikungunya outbreaks, many myths and false beliefs make the rounds, especially on social media and in communities lacking reliable health education.
Here are some common myths—and the facts to correct them:
- Myth: Chikungunya is contagious between people.
Fact: It’s not spread through casual contact, touching, or breathing the same air. Only mosquito bites from infected mosquitoes transmit it. - Myth: Chikungunya only affects poor countries.
Fact: It can affect anyone, anywhere, especially as Aedes mosquitoes expand their range. - Myth: Drinking papaya leaf juice cures Chikungunya.
Fact: While some herbal remedies can support symptom relief, they don’t cure the virus. Always seek medical advice. - Myth: Once you have Chikungunya, you’re sick forever.
Fact: Most people recover in 1–2 weeks. Chronic symptoms are possible but not guaranteed.
Believing these myths can delay treatment or prevent people from taking necessary precautions. Accurate information is key to staying safe and healthy.
Educating Communities About the Virus
Health education is critical in the fight against Chikungunya. When communities are informed, they are better equipped to take action—whether it’s cleaning up breeding sites, using repellents, or recognizing symptoms early.
Public health officials should use multiple communication channels—TV, radio, posters, school programs, social media—to reach different segments of the population. Educational campaigns should:
- Highlight mosquito prevention tips.
- Clarify differences between Chikungunya, dengue, and Zika.
- Provide instructions on what to do if symptoms arise.
- Encourage community cleanup events.
Engaging local leaders, school teachers, and religious figures can also help spread messages effectively, especially in rural areas. Health literacy saves lives—and every well-informed person becomes a line of defense against the disease.
Conclusion
Chikungunya may not be as deadly as some other mosquito-borne diseases, but it leaves a lasting impact on individuals, families, and healthcare systems. The intense joint pain, fatigue, and chronic effects it causes can be life-altering, especially in vulnerable populations.
With climate change expanding the mosquito’s habitat, and urbanization contributing to breeding grounds, the threat of Chikungunya is growing globally. But knowledge is power. By understanding how the virus spreads, recognizing symptoms early, and taking preventative steps, we can protect ourselves and our communities.
From using mosquito repellents and eliminating stagnant water to educating others and supporting scientific research, everyone has a role to play in stopping the spread of Chikungunya. As science advances toward vaccine development, continued vigilance, preparedness, and community cooperation remain our strongest weapons.
Frequently Asked Questions (FAQs)
- Can Chikungunya be spread through kissing or physical contact?
No. Chikungunya cannot be transmitted through human-to-human contact. It spreads only through the bite of an infected mosquito. - How long does it take to recover from Chikungunya?
Most people recover within 1–2 weeks. However, some may experience joint pain and fatigue for months, especially older adults. - Is there a cure for Chikungunya?
There’s no specific cure. Treatment focuses on relieving symptoms like pain, fever, and swelling through supportive care. - Can you get Chikungunya more than once?
Unlikely. Most people develop immunity after the first infection, which generally provides lifelong protection against the virus.
5. What’s the best way to avoid getting Chikungunya?
Prevent mosquito bites by using repellents, wearing protective clothing, and eliminating standing water where mosquitoes breed.

Leave a Reply